Trends in Chiropractic Care and Physical Rehabilitation Use Among Adults with Low Back Pain in the United States, 2002 to 2018
Trends in Chiropractic Care and Physical Rehabilitation Use Among Adults with Low Back Pain in the United States, 2002 to 2018
SOURCE: J Gen Intern Med. 2023 (Oct 19); 39 (4): 578–586
Eric J Roseen • Kushang V Patel • Rachel Ward • Xinyao de Grauw
Steven J Atlas • Stephen Bartels • Julie J Keysor • Jonathan F Bean
Section of General Internal Medicine,
Department of Medicine, Boston University,
Chobanian & Avedision School of Medicine and
Boston Medical Center,
Boston, MA, USA.
Background While nonpharmacologic treatments are increasingly endorsed as first-line therapy for low back pain (LBP) in clinical practice guidelines, it is unclear if use of these treatments is increasing or equitable.
Objective Examine national trends in chiropractic care and physical rehabilitation (occupational/physical therapy (OT/PT)) use among adults with LBP.
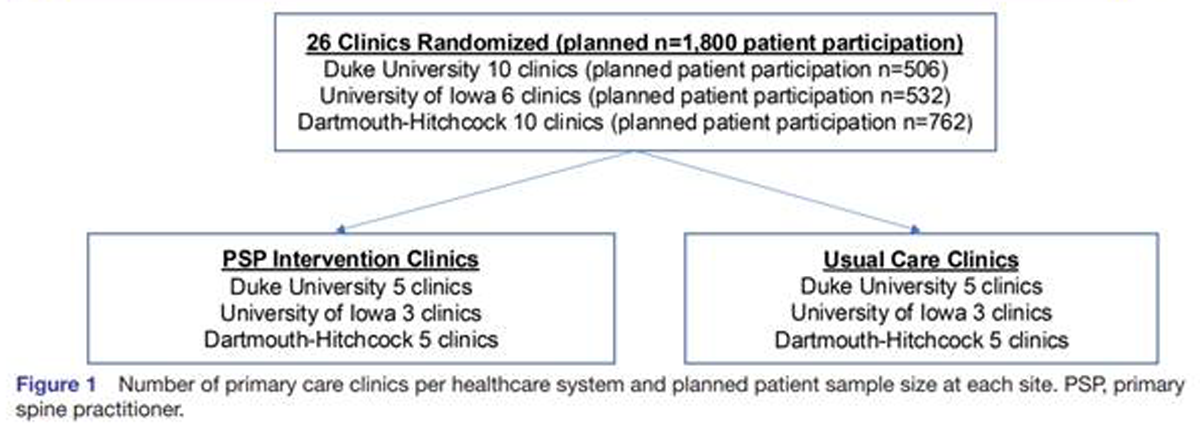
Design/Setting Serial cross-sectional analysis of the National Health Interview Survey, 2002 to 2018.
Participants 146,087 adults reporting LBP in prior 3 months.
Methods We evaluated the association of survey year with chiropractic care or OT/PT use in prior 12 months. Logistic regression with multilevel linear splines was used to determine if chiropractic care or OT/PT use increased after the introduction of clinical guidelines. We also examined trends in use by age, sex, race, and ethnicity. When trends were similar over time, we present differences by these demographic characteristics as unadjusted ORs using data from all respondents.
Results Between 2002 and 2018, less than one-third of adults with LBP reported use of either chiropractic care or OT/PT. Rates did not change until 2016 when uptake increased with the introduction of clinical guidelines (2016–2018 vs 2002–2015, OR` =` 1.15; 95% CI: 1.10–1.19). Trends did not differ significantly by sex, race, or ethnicity (p for interactions` >` 0.05). Racial and ethnic disparities in chiropractic care or OT/PT use were identified and persisted over time. For example, compared to non-Hispanic adults, either chiropractic care or OT/PT use was lower among Hispanic adults (combined OR` =` 0.62, 95% CI: 0.65–0.73). By contrast, compared to White adults, Black adults had similar OT/PT use (OR` =` 0.98; 95% CI: 0.94–1.03) but lower for chiropractic care use (OR` =` 0.50; 95% CI: 0.47–0.53).
There are more articles like this @