Development, Validation and Use of Custom Software for the Analysis of Pain Trajectories
Development, Validation and Use of Custom Software for the Analysis of Pain Trajectories
SOURCE: Sci Rep 2024 (Aug 12); 14 (1): 18719
| OPEN ACCESS |
M. R. van Ittersum • A. de Zoete • M. Rubinstein • Al-Madfai
A. Kongsted • P. McCarthy
Chiropractie Groesbeek,
Nijmeegsebaan 32, 6561 KG,
Groesbeek, The Netherlands.
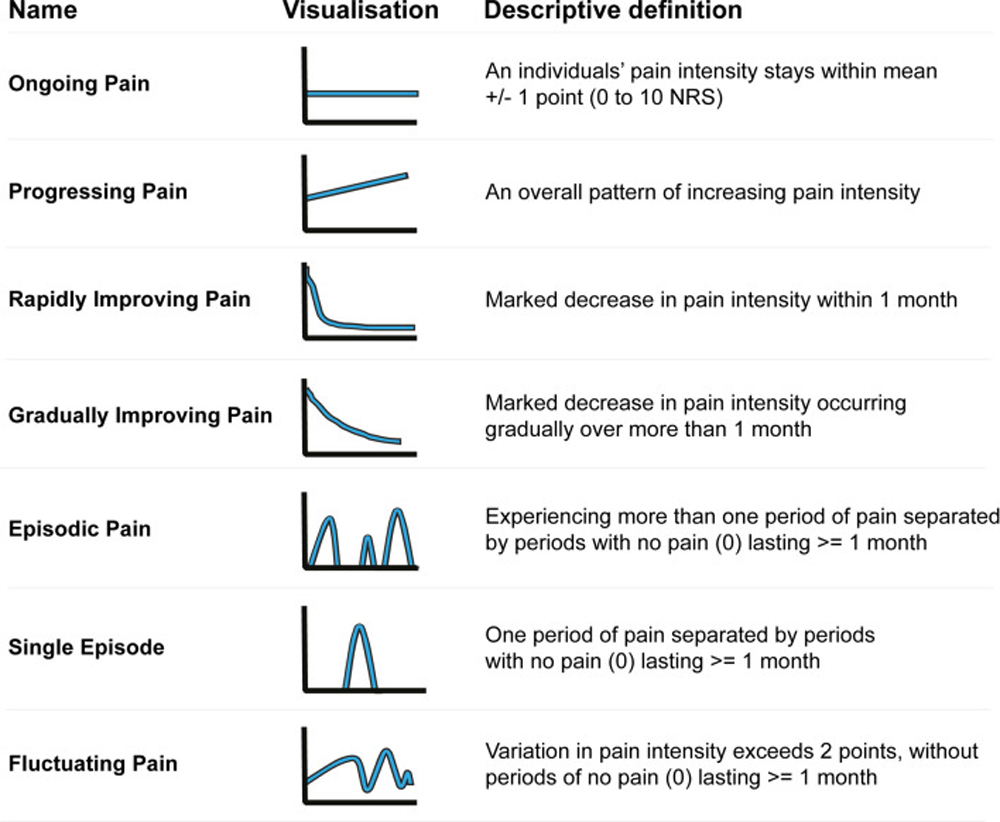
In chronic musculoskeletal conditions, the prognosis tends to be more informative than the diagnosis for the future course of the disease. Many studies have identified clusters of patients who seemingly share similar pain trajectories. In a dataset of low back pain (LBP) patients, pain trajectories have been identified, and distinct trajectory types have been defined, making it possible to create pattern recognition software that can classify patients into respective pain trajectories reflecting their condition. It has been suggested that the classification of pain trajectories may create clinically meaningful subgroups of patients in an otherwise heterogeneous population of patients with LBP. A software tool was created that combined the ability to recognise the pain trajectory of patients with a system that could create subgroups of patients based on their characteristics. This tool is primarily meant for researchers to analyse trends in large heterogeneous datasets without large losses of data. Prospective analysis of pain trajectories is not directly helpful for clinicians. However, the tool might aid in the identification of patient characteristics which have predictive capabilities of the most likely trajectory a patient might experience in the future. This will help clinicians to tailor their advice and treatment for a specific patient.
Subject terms: Data mining, Chronic pain, Prognosis
From the FULL TEXT Article:
Introduction
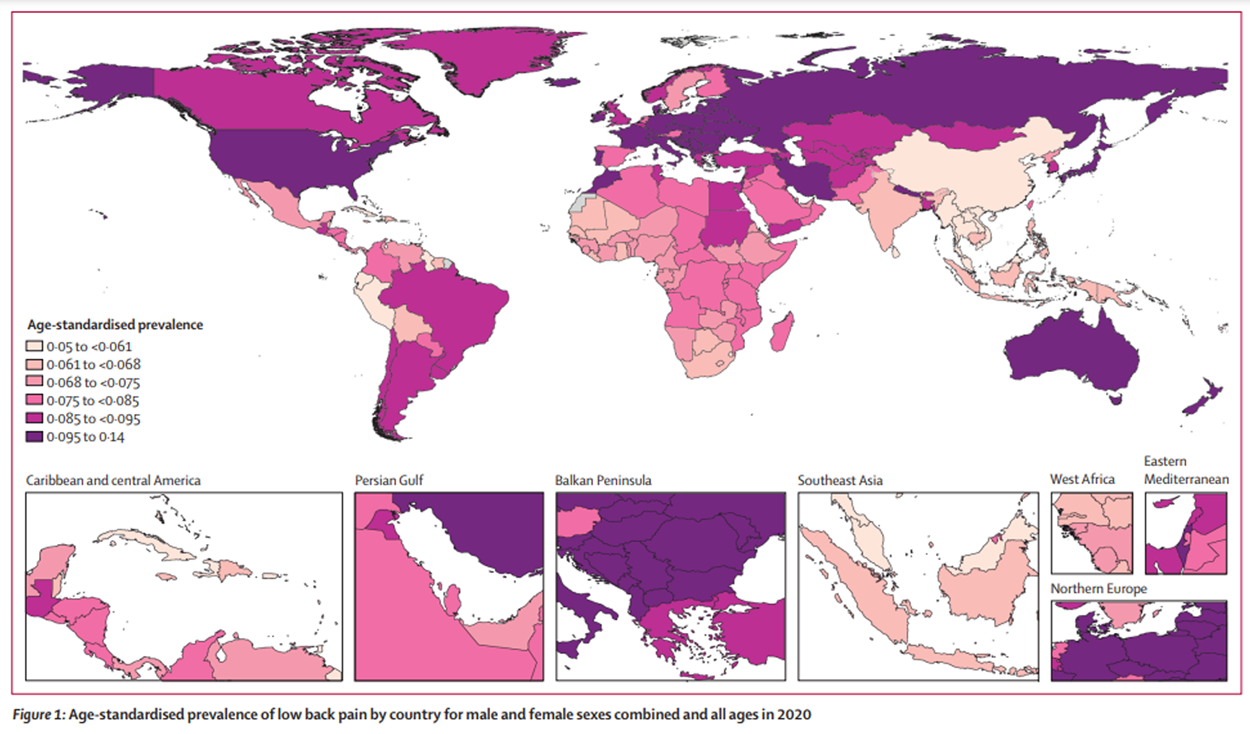
In chronic musculoskeletal diseases, diagnosis alone is often insufficient to inform patients and clinicians about the future course of the disease. [1] Most chronic musculoskeletal diseases, such as low back pain (LBP), are caused by a complex combination of biological, psychological, social, and genetic factors that influence the course of the disease. [2] It is therefore argued that prognosis, which considers all of these elements, might be a better framework to inform patients and clinicians about the likely course of the disease. [1]
There are more articles like this @