Cost of Chiropractic Versus Medical Management of Adults with Spine-related Musculoskeletal Pain: A Systematic Review
Cost of Chiropractic Versus Medical Management of Adults with Spine-related Musculoskeletal Pain: A Systematic Review
SOURCE: Chiropractic & Manual Therapies 2024 (Mar 6); 32: 8
| OPEN ACCESS |
Ronald Farabaugh • Cheryl Hawk • Dave Taylor • Clinton Daniels • Claire Noll • Mike Schneider • John McGowan • Wayne Whalen • Ron Wilcox • Richard Sarnat • Leonard Suiter • James Whedon
American Chiropractic Association,
2008 St. Johns Avenue,
Highland Park, Illiois. 60035
Arlington, VA, USA.
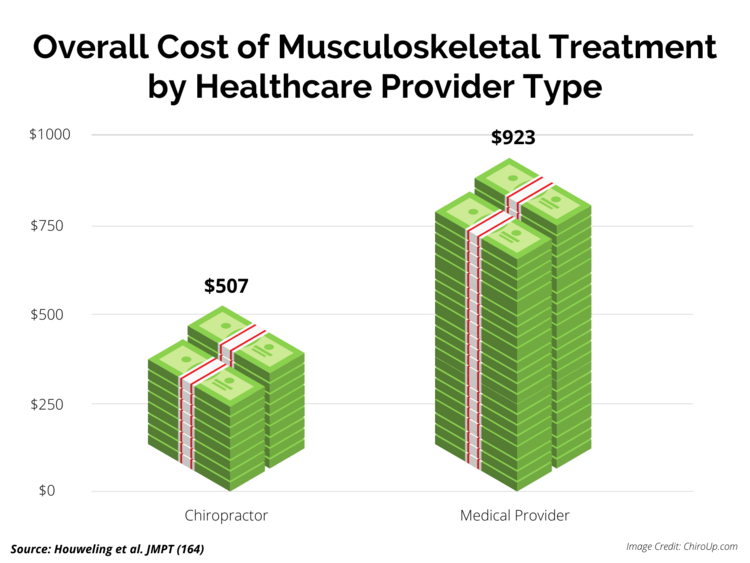
FROM: Houweling, JMPT 2015
Background: The cost of spine-related pain in the United States is estimated at $134.5 billion. Spinal pain patients have multiple options when choosing healthcare providers, resulting in variable costs. Escalation of costs occurs when downstream costs are added to episode costs of care. The purpose of this review was to compare costs of chiropractic and medical management of patients with spine-related pain.
Methods: A Medline search was conducted from inception through October 31, 2022, for cost data on U.S. adults treated for spine-related pain. The search included economic studies, randomized controlled trials and observational studies. All studies were independently evaluated for quality and risk of bias by 3 investigators and data extraction was performed by 3 investigators.
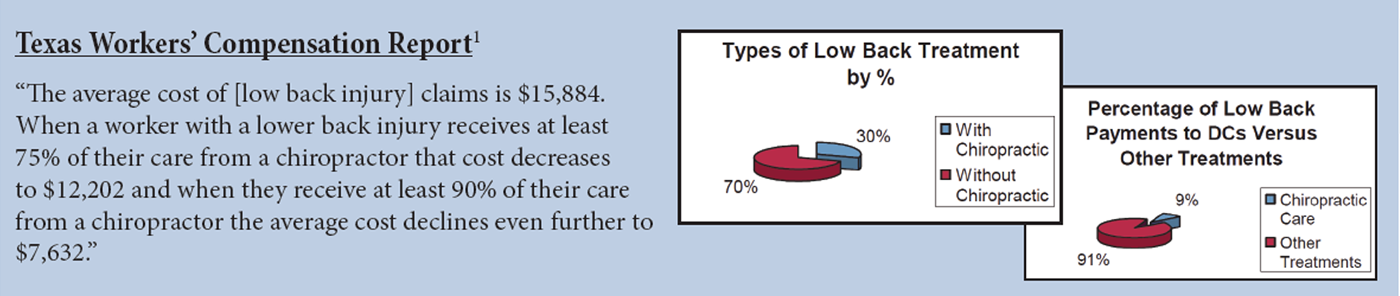
Results: The literature search found 2256 citations, of which 93 full-text articles were screened for eligibility. Forty-four studies were included in the review, including 26 cohort studies, 17 cost studies and 1 randomized controlled trial. All included studies were rated as high or acceptable quality. Spinal pain patients who consulted chiropractors as first providers needed fewer opioid prescriptions, surgeries, hospitalizations, emergency department visits, specialist referrals and injection procedures.
There is more like this @
COST-EFFECTIVENESS Section and the
SPINAL PAIN MANAGEMENT Section and the