Chiropractic Care for Workers with Low Back Pain
Chiropractic Care for Workers with Low Back Pain
SOURCE: Workers Compensation Research Institute (May 17, 2022)
Dongchun Wang, Kathryn Mueller, Randall Lea, M.D., Donald R. Murphy
Related Topics: Medical Costs, Outcomes for Injured Workers, Physical Medicine, Utilization
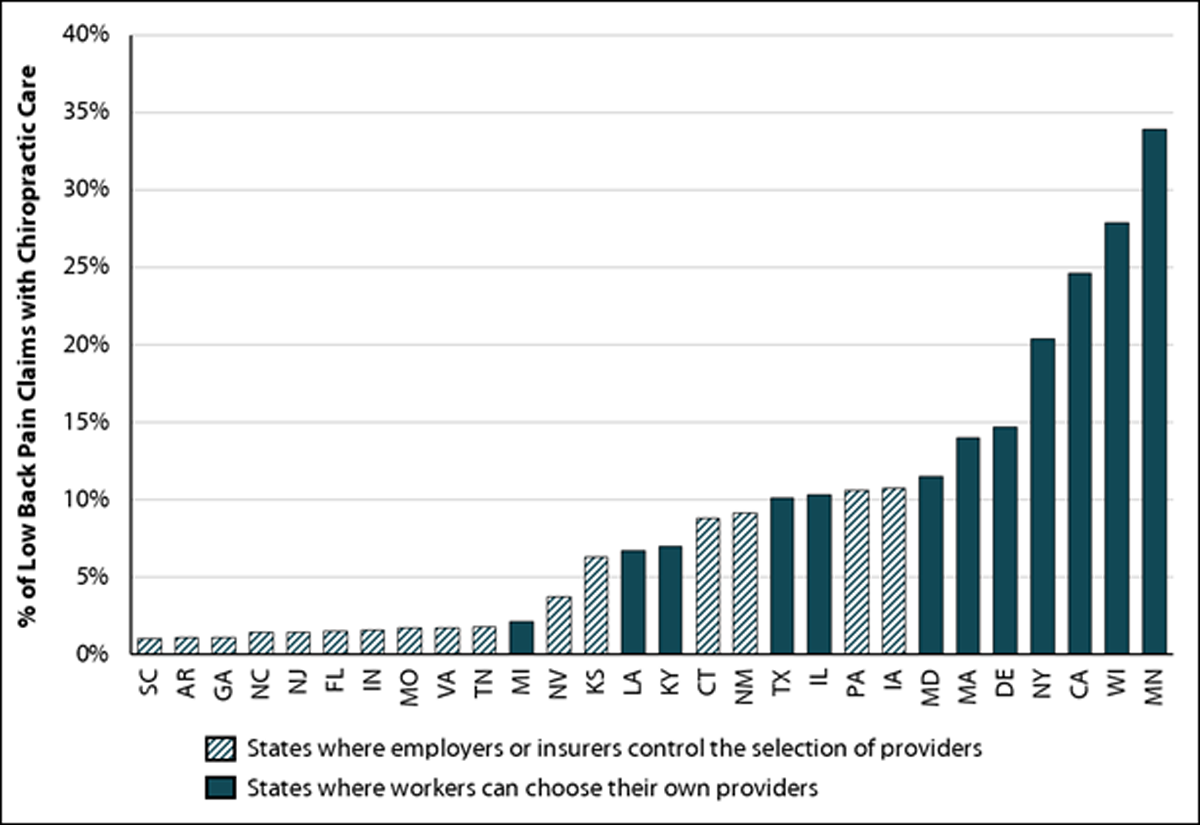
Cambridge, MA, May 17, 2022 — Today, the Workers Compensation Research Institute (WCRI) announced the release of a new study on chiropractic care for low back pain. The study reveals substantial variation in the use of chiropractic care across 28 states and offers insights into the patterns and outcomes of chiropractic care.
“Chiropractors often participate in the delivery of physical medicine services for low back pain, but few workers received chiropractic care in states where employers or insurers control the selection of providers,” said John Ruser, WCRI’s president and CEO. “This study will be helpful for policymakers and stakeholders who are interested in re-evaluating the role of chiropractors, especially those who have been adopting evidence-based practices and contributing to cost-effective care.”
This study, Chiropractic Care for Workers with Low Back Pain, describes the prevalence of chiropractic care and provider patterns of physical medicine treatment for workers with low back pain. It provides some evidence as to how different provider patterns of physical medicine treatment are associated with variations in overall medical and indemnity costs, and the duration of temporary disability. The study also looks at the utilization of medical services, including magnetic imaging studies, opioid prescriptions, and pain management injections.
The following is a sample of the study’s key findings:
There are more articles like this @