Association Between Spinal Manipulative Therapy and Lumbar Spine Reoperation After Discectomy: A Retrospective Cohort Study
SOURCE: BMC Musculoskelet Disord 2024 (Jan 10); 25 (1): 46
Robert J. Trager, Jordan A. Gliedt Collin M. Labak,Clinton J. Daniels, and Jeffery A. Dusek
Connor Whole Health,
University Hospitals Cleveland Medical Center,
Cleveland, OH, USA.
Background: Patients who undergo lumbar discectomy may experience ongoing lumbosacral radiculopathy (LSR) and seek spinal manipulative therapy (SMT) to manage these symptoms. We hypothesized that adults receiving SMT for LSR at least one year following lumbar discectomy would be less likely to undergo lumbar spine reoperation compared to matched controls not receiving SMT, over two years’ follow-up.
Methods: We searched a United States network of health records (TriNetX, Inc.) for adults aged ≥ 18 years with LSR and lumbar discectomy ≥ 1 year previous, without lumbar fusion or instrumentation, from 2003 to 2023. We divided patients into two cohorts: (1) chiropractic SMT, and (2) usual care without chiropractic SMT. We used propensity matching to adjust for confounding variables associated with lumbar spine reoperation (e.g., age, body mass index, nicotine dependence), calculated risk ratios (RR), with 95% confidence intervals (CIs), and explored cumulative incidence of reoperation and the number of SMT follow-up visits.
Results: Following propensity matching there were 378 patients per cohort (mean age 61 years). Lumbar spine reoperation was less frequent in the SMT cohort compared to the usual care cohort (SMT: 7%; usual care: 13%), yielding an RR (95% CIs) of 0.55 (0.35-0.85; P = 0.0062). In the SMT cohort, 72% of patients had ≥ 1 follow-up SMT visit (median = 6).
There are more articles like this @
Conclusions: This study found that adults experiencing LSR at least one year after lumbar discectomy who received SMT were less likely to undergo lumbar spine reoperation compared to matched controls not receiving SMT. While these findings hold promise for clinical implications, they should be corroborated by a prospective study including measures of pain, disability, and safety to confirm their relevance. We cannot exclude the possibility that our results stem from a generalized effect of engaging with a non-surgical clinician, a factor that may extend to related contexts such as physical therapy or acupuncture.
Registration: Open Science Framework ( https://osf.io/vgrwz ).
Keywords: Keywords: Chiropractic; Intervertebral disc; Lumbar vertebrae; Lumbosacral region; Spinal manipulation; Surgical decompression.
From the FULL TEXT Article:
Background
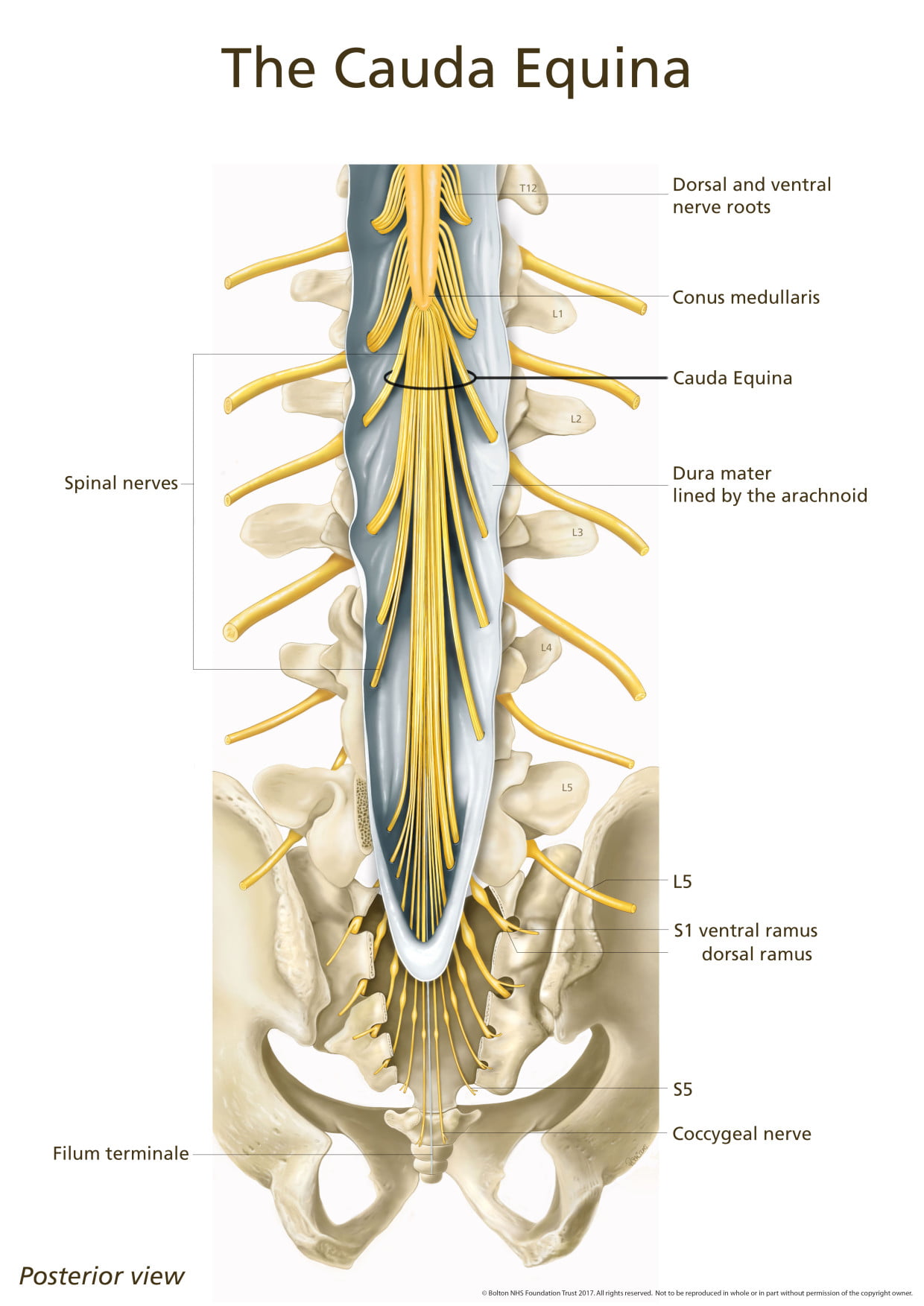
Lumbar discectomy is a surgical procedure often performed to remove herniated intervertebral disc material to alleviate refractory lower extremity pain, numbness, or weakness. [1] These symptoms, referred to in constellation as lumbosacral radiculopathy (LSR), may recur or persist following discectomy and prompt additional surgery (i.e., reoperation). [1–4] Reoperation after lumbar discectomy is common, with a reported rate of 6 to 12%. [1–4] Reoperation within three months following discectomy is typically performed to address acute postoperative complications including hematoma or infection. [2, 5] However, the majority of reoperations are performed after three months to address recurrent same-level disc herniation. [2, 6]
About 20% of patients undergoing lumbar discectomy have continued or recurrent LSR at one year after surgery [7]. For such cases, first-line treatments often consist of pain medications, spinal injections, cognitive behavioral therapy, and physical therapy exercises. [8, 9] In contrast, spinal reoperations are considered a final option due to generally having a lower success rate compared to primary surgeries. [8] In general, there is no consensus on the most appropriate care strategy for such patients. [9]
Spinal manipulative therapy (SMT) has emerged as a potential treatment for those with ongoing LSR following spine surgery [10, 11]. Among patients receiving SMT from chiropractors, the primary providers of SMT in the United States (US [12], approximately 11% of patients have a history of spine surgery. [10] Case series have reported improvements in pain and disability among patients with previous spine surgery receiving SMT. [13–15] However, to our knowledge, no studies have yet examined the association between SMT and spinal reoperation.
This study investigated the association between SMT and reoperation among patients experiencing LSR at least one year after lumbar discectomy. Considering the literature gap on effective treatments for LSR after discectomy and the limited but encouraging findings regarding SMT in this population [13–15], we hypothesized that adults receiving SMT for LSR at least one year after lumbar discectomy would be less likely to undergo reoperation compared to matched controls receiving usual care without SMT.



Leave A Comment