Swiss Chiropractic Practice-based Research Network and Musculoskeletal Pain Cohort Pilot Study: Protocol of a Nationwide Resource to Advance Musculoskeletal Health Services Research
Swiss Chiropractic Practice-based Research Network and Musculoskeletal Pain Cohort Pilot Study: Protocol of a Nationwide Resource to Advance Musculoskeletal Health Services Research
SOURCE: BMJ Open 2022 (Jul 13); 12 (7): e059380
| OPEN ACCESS |
Rahim Lalji, Léonie Hofstetter, Alice Kongsted, Viktor von Wyl, Milo A Puhan, and Cesar A Hincapié
Department of Chiropractic Medicine,
Balgrist University Hospital and University of Zurich,
Zurich, Switzerland.
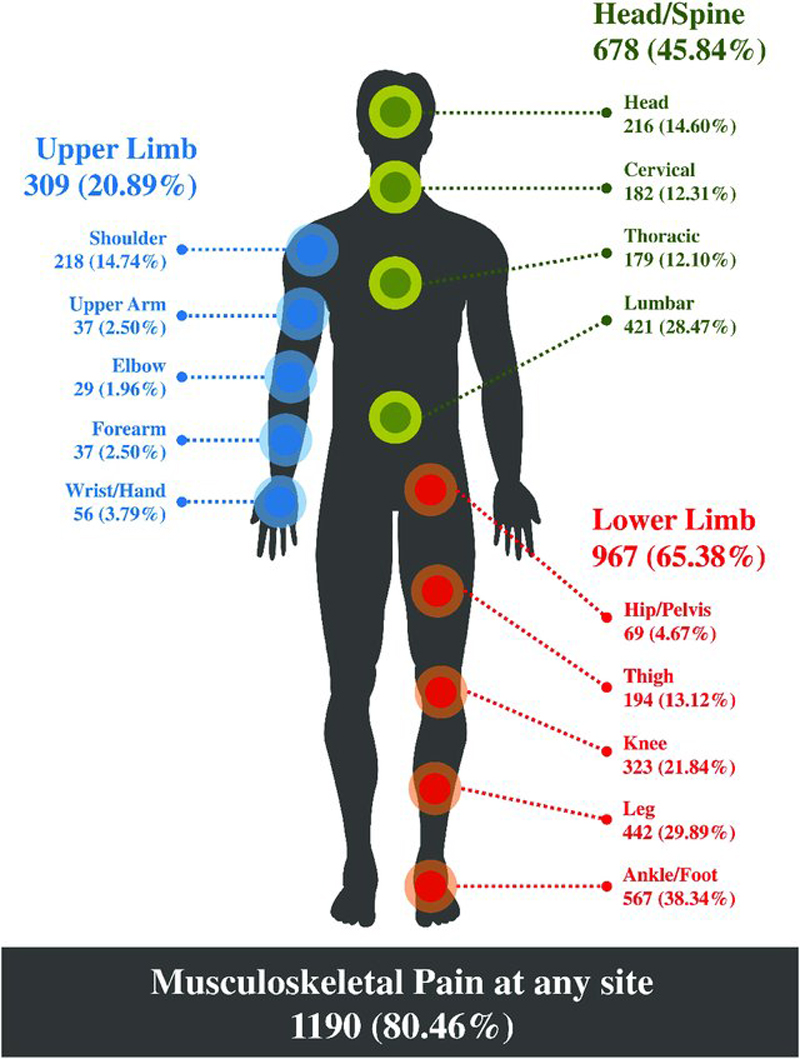
Introduction: Musculoskeletal (MSK) pain conditions, a leading cause of global disability, are usually first managed in primary care settings such as medical, physiotherapy, and chiropractic community-based practices. While chiropractors often treat MSK conditions, there is limited real-world evidence on the topic of health service outcomes among patients receiving this type of care. A nationwide Swiss chiropractic practice-based research network (PBRN) and MSK pain patient cohort study will have potential to monitor the epidemiological trends of MSK pain conditions and contribute to healthcare quality improvement. The primary aims of this protocol are to (1) describe the development of an MSK-focused PBRN within the Swiss chiropractic setting, and (2) describe the methodology of the first nested study to be conducted within the PBRN-an observational prospective patient cohort pilot study.
Methods and analysis: This initiative is conceptualised with two distinct phases. Phase I focuses on the development of the Swiss chiropractic PBRN, and will use a cross-sectional design to collect information from chiropractic clinicians nationwide. Phase II will recruit consecutive patients aged 18 years or older with MSK pain from community-based chiropractic practices participating in the PBRN into a prospective chiropractic cohort pilot study. All data collection will occur through electronic surveys offered in the three Swiss official languages (German, French, Italian) and English. Surveys will be provided to patients prior to their initial consultation in clinics, 1 hour after initial consultation, and at 2, 6 and 12 weeks after initial consultation.
Ethics and dissemination: Ethics approval has been obtained from the independent research ethics committee of Canton Zurich (BASEC-Nr: 2021-01479). Informed consent will be obtained electronically from all participants.
There are more articles like this @ our: