Self-management at the Core of Back Pain Care:
10 Key Points for Clinicians
Self-management at the Core of Back Pain Care:
10 Key Points for Clinicians
SOURCE: Braz J Phys Ther 2021 (Jul); 25 (4): 396–406
Alice Kongsted, Inge Ris, Per Kjaer, Jan Hartvigsen
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmarkm
Odense M, Denmark;
Chiropractic Knowledge Hub,
Odense M, Denmark.
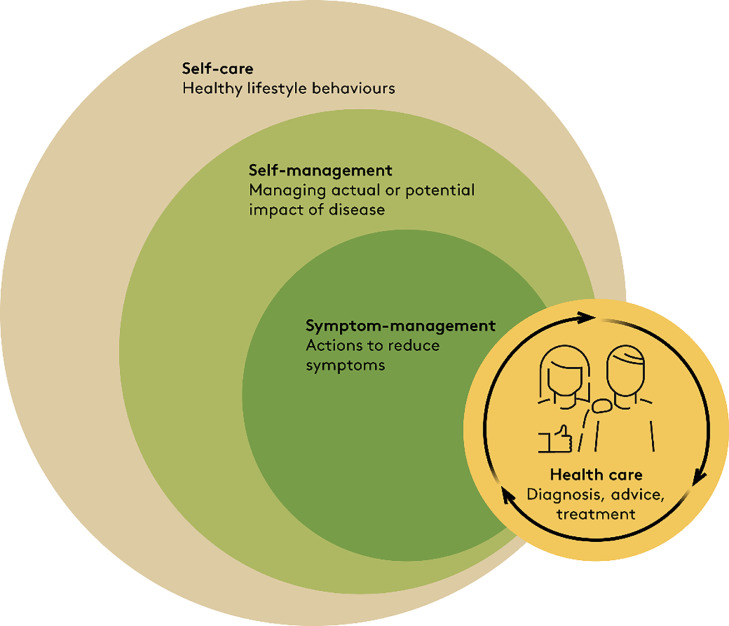
Background: A paradigm shift away from clinician-led management of people with chronic disorders to people playing a key role in their own care has been advocated. At the same time, good health is recognised as the ability to adapt to changing life circumstances and to self-manage. Under this paradigm, successful management of persistent back pain is not mainly about clinicians diagnosing and curing patients, but rather about a partnership where clinicians help individuals live good lives despite back pain.
Objective: In this paper, we discuss why there is a need for clinicians to engage in supporting self-management for people with persistent back pain and which actions clinicians can take to integrate self-management support in their care for people with back pain.
Discussion: People with low back pain (LBP) self-manage their pain most of the time. Therefore, clinicians and health systems should empower them to do it well and provide knowledge and skills to make good decisions related to LBP and general health. Self-management does not mean that people are alone and without health care, rather it empowers people to know when to consult for diagnostic assessment, symptom relief, or advice. A shift in health care paradigm and clinicians’ roles is not only challenging for individual clinicians, it requires organisational support in clinical settings and health systems. Currently, there is no clear evidence showing how exactly LBP self-management is most effectively supported in clinical practice, but core elements have been identified that involve working with cognitions related to pain, behaviour change, and patient autonomy.
There is more like this @ our: