Implementation of the American- College of Physicians Guideline for Low Back Pain (IMPACt-LBP):
Protocol for a Healthcare Systems Embedded Multisite Pragmatic Cluster-randomized Trialal
Implementation of the American- College of Physicians Guideline for Low Back Pain (IMPACt-LBP):
Protocol for a Healthcare Systems Embedded Multisite Pragmatic Cluster-randomized Trial
SOURCE: BMJ Open 2025 (Mar 26); 15 (3): e097133
Adam P Goode • Christine Goertz • Hrishikesh Chakraborty • Stacie A Salsbury • Samuel Broderick
Barcey T Levy • Kelley Ryan • Sharon Settles • Shoshana Hort • Rowena J Dolor, et al.
Duke University School of Medicine,
Durham, North Carolina, USA
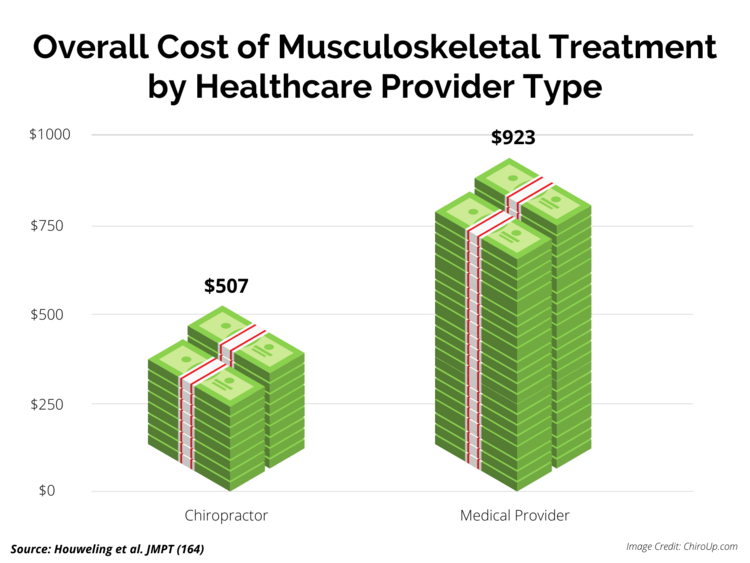
Introduction: Low back pain (LBP) is a key source of medical costs and disability, impacting over 31 million Americans at any given time and resulting in US$100-US$200 billion per year in total healthcare costs. LBP is one of the leading causes of ambulatory care visits to US physicians; problematically, these visits often result in treatments such as opioids, surgery or advanced imaging that can lead to more harm than benefit. The American College of Physicians (ACP) Guideline for Low Back Pain recommends patients receive non-pharmacological interventions as a first-line treatment. Roadmaps exist for multidisciplinary collaborative care that include well-trained primary contact clinicians with specific expertise in the treatment of musculoskeletal conditions, such as physical therapists and doctors of chiropractic, as first-line providers for LBP. These clinicians, sometimes referred to as primary spine practitioners (PSPs) routinely employ many of the non-pharmacological approaches recommended by the ACP guideline, including spinal manipulation and exercise. Important foundational work has demonstrated that such care is feasible and safe, and results in improved physical function, less pain, fewer opioid prescriptions and reduced utilisation of healthcare services. However, this treatment approach for LBP has yet to be widely implemented or tested in a multisite clinical trial in real-world practice.
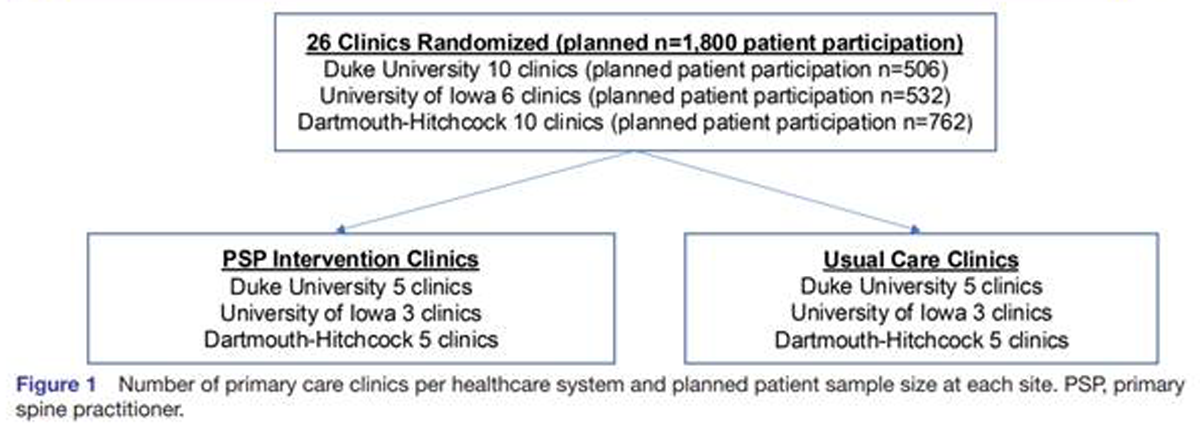
Methods and analysis: The Implementation of the American College of Physicians Guideline for Low Back Pain trial is a health system-embedded pragmatic cluster-randomised trial that will examine the effect of offering initial contact with a PSP compared with usual primary care for LBP. Twenty-six primary care clinics within three healthcare systems were randomised 1:1 to PSP intervention or usual primary care.
Primary outcomes are pain interference and physical function using the Patient-Reported Outcomes Measurement Information System Short Forms collected via patient self-report among a planned sample of 1800 participants at baseline, 1, 3 (primary end point), 6 and 12 months. A subset of participants enrolled early in the trial will also receive a 24-month assessment. An economic analysis and analysis of healthcare utilisation will be conducted as well as an evaluation of the patient, provider and policy-level barriers and facilitators to implementing the PSP model using a mixed-methods process evaluation approach.
Ethics and dissemination: The study received ethics approval from Advarra, Duke University, Dartmouth Health and the University of Iowa Institutional Review Boards. Study data will be made available on completion, in compliance with National Institutes of Health data sharing policies.
There are more articles like this @