Our Blog is a Tool. Learn How to Use It Now
Our Blog is a Tool.
Learn How to Use It Now
A Chiro.Org Editorial
Every Blog post is an announcement of new material that was just added to one of our many Sections.
I have been compiling (and archiving) peer-reviewed articles since early 1996, and to date we have thousands of Abstracts, and many hundreds of Full-Text articles on a wide variety of subjects.
When enough material, relating to a particular topic was collected,
it was gathered into a new Topical Page in one of our many Sections.
Each Topical page is located in the Section most associated with that topic.
Thus, our Attention Deficit Page is located (is a part of) our Pediatrics Section You get the idea.
Almost ALL of our Sections contain some, or many Topical collections.
The LINKS Section is the most extreme example,
because it contains 86 different topical pages.
All of the following are “active” Sections that are constantly adding new (and important) materials:
Alternative Healing Abstracts
Case Studies
Chiropractic Assistants
Chiropractic Research
Chronic Neck Pain
Conditions That Respond Well
Cost-Effectiveness of Chiropractic
Documentation
Global Burden of Disease
Headache and Chiropractic
Initial Provider/First Contact and Chiropractic
The LINKS
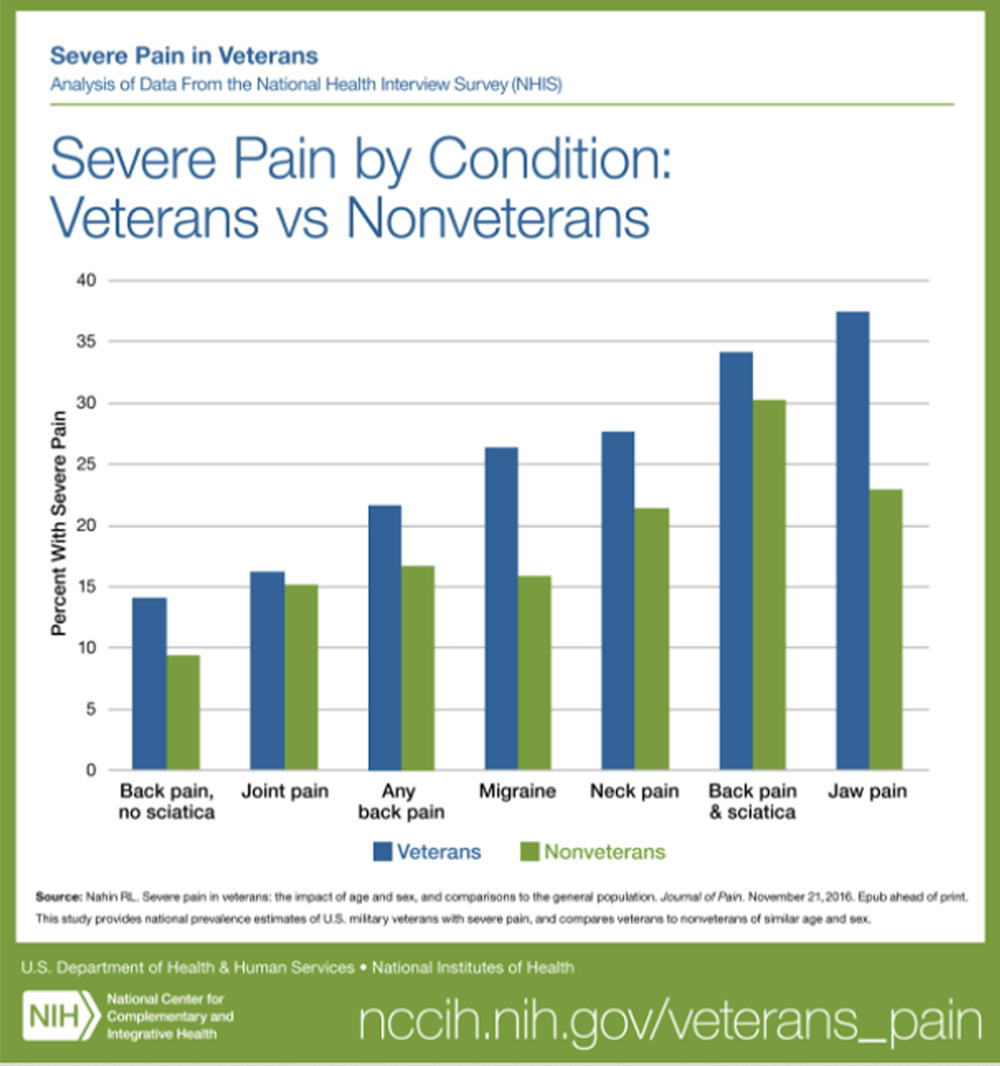
Low Back Pain and Chiropractic
Medicare Info
Non-pharmacologic Therapy and Chiropractic
Nutrition
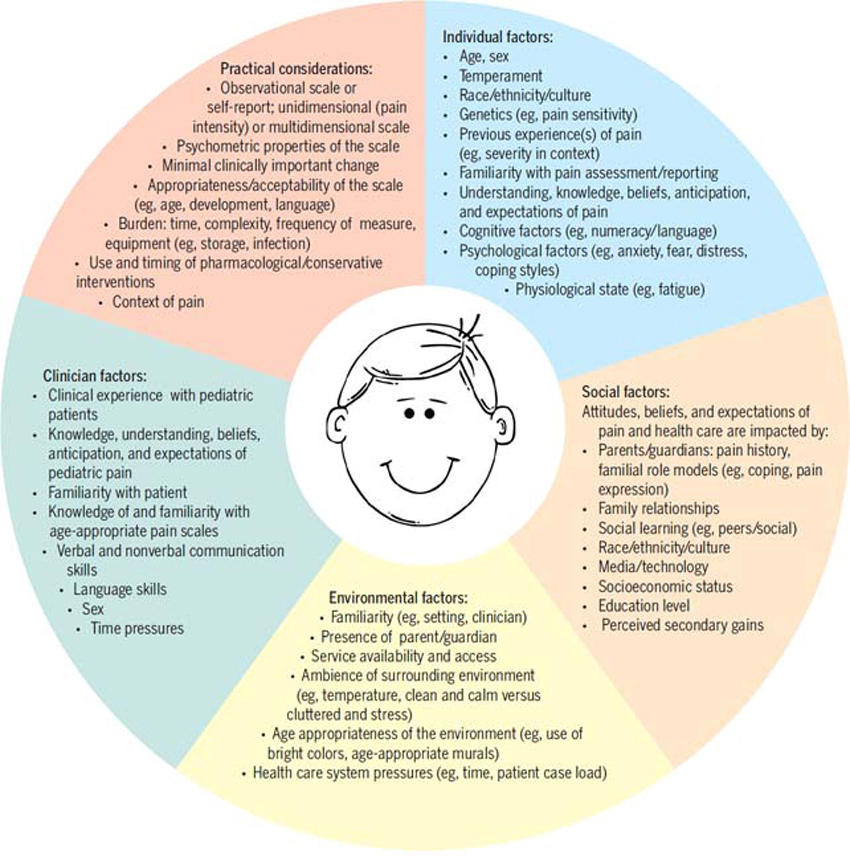
Pediatrics
Radiology
The SEARCH Section
Stroke and Chiropractic
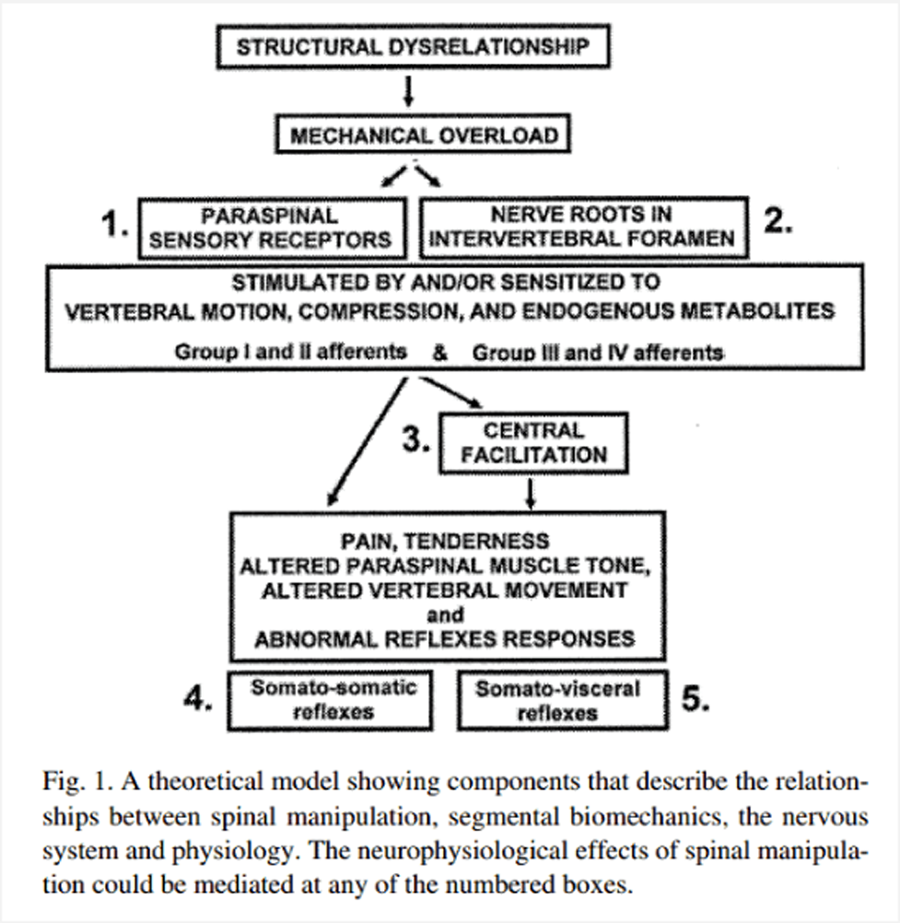
What is the Chiropractic Subluxation?
Whiplash and Chiropractic
These other Sections are “archival” in nature, and contain valuable tools:
ChiroZine
Free Images
New DC’s
Office Forms
R.C. Schafer’s Rehab Monographs
The Wilk Antitrust Lawsuit
How Blog Posts Work
The following is a Graphic “screen grab” of a Blog Post from our Home Page.
(more…)