Measuring Musculoskeletal Pain in Infants, Children, and Adolescents
Measuring Musculoskeletal Pain in Infants, Children, and Adolescents
SOURCE: J Orthop Sports Phys Ther 2017 (Oct); 47 (10): 712–730
| OPEN ACCESS |
Zoe A. Michaleff, BAppSc (Phty), PhD, Steven J. Kamper, BSc, BAppSc, PhD, et al.
Primary Care Centre,
Research Institute for Primary Care and Health Sciences,
Keele University,
Keele, Staffordshire
ST5 5BG United Kingdom.
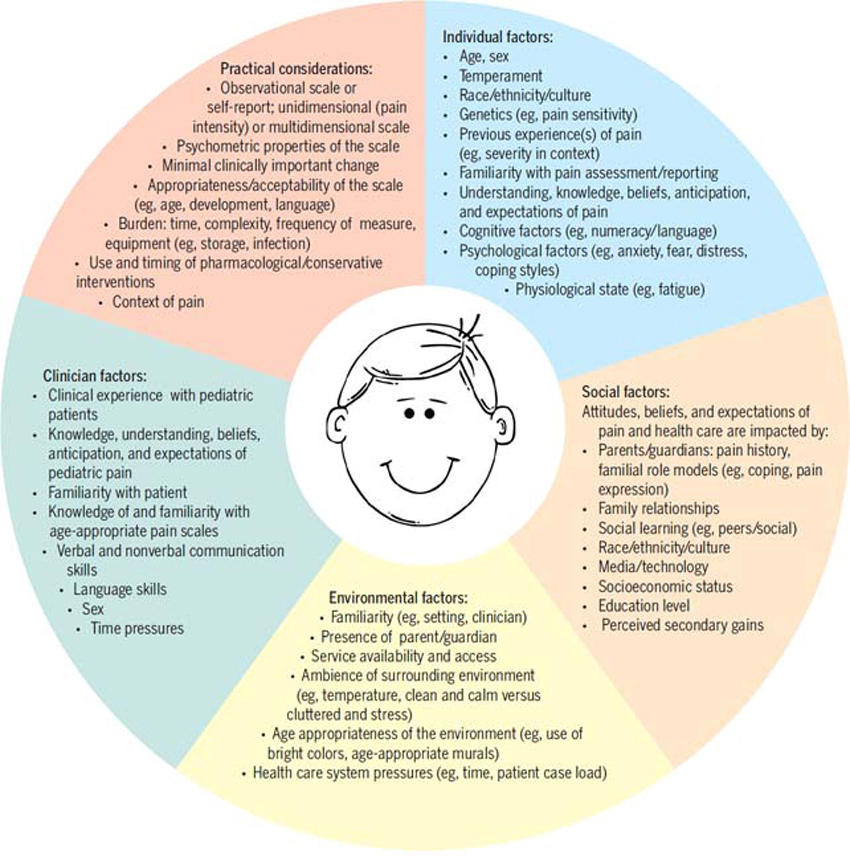
Accurate, reliable, and timely assessment of pain is critical for effective management of musculoskeletal pain conditions. The assessment of pain in infants, children, and adolescents with and without cognitive impairment can be particularly challenging to clinicians for a number of reasons, including factors related to the consultation (eg, heterogeneous patient population, time constraints), the clinician (eg, awareness/knowledge of available pain scales), standardized assessment scales (eg, availability, psychometric properties, and application of each scale), the patient (eg, developmental stage, ability to communicate), and the context in which the interaction took place (eg, familiarity with the setting and physiological and psychological state).
As a result, pain is frequently not assessed or measured during the consultation and, in many instances, underestimated and undertreated in this population. The purpose of this article is to provide clinicians with an overview of scales that may be used to measure pain in infants, children, and adolescents.
There are more articles like this @ our: