Awareness of Axial Spondyloarthritis Among Chiropractors
Awareness of Axial Spondyloarthritis Among Chiropractors and Osteopaths: Findings From a UK Web-based Survey
SOURCE: Rheumatol Adv Pract. 2019 (Sep 30)
Cee Y Yong, Jill Hamilton, Jatinder Benepal, Katie Griffiths, Zoë E Clark, Amanda Rush, Raj Sengupta, Jane Martindale, and Karl Gaffney
Department of Rheumatology,
North West Anglia NHS Foundation Trust,
Huntingdon.
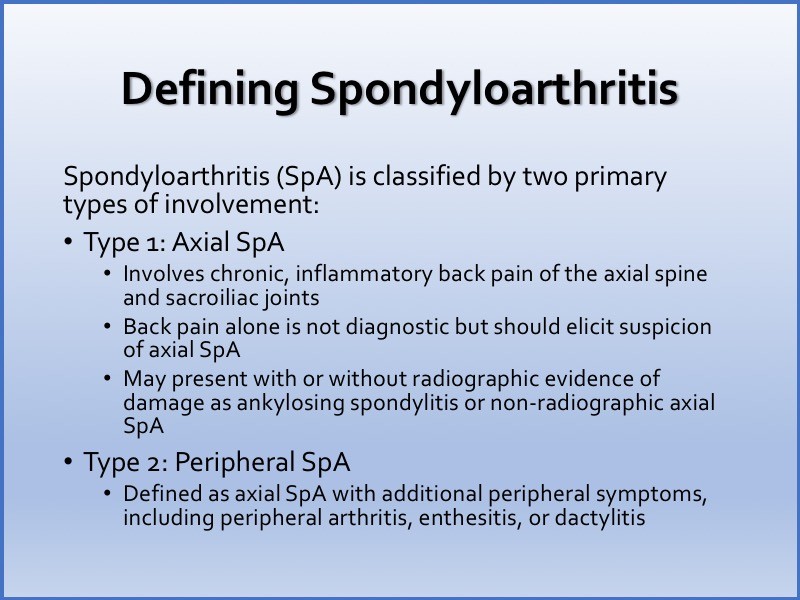
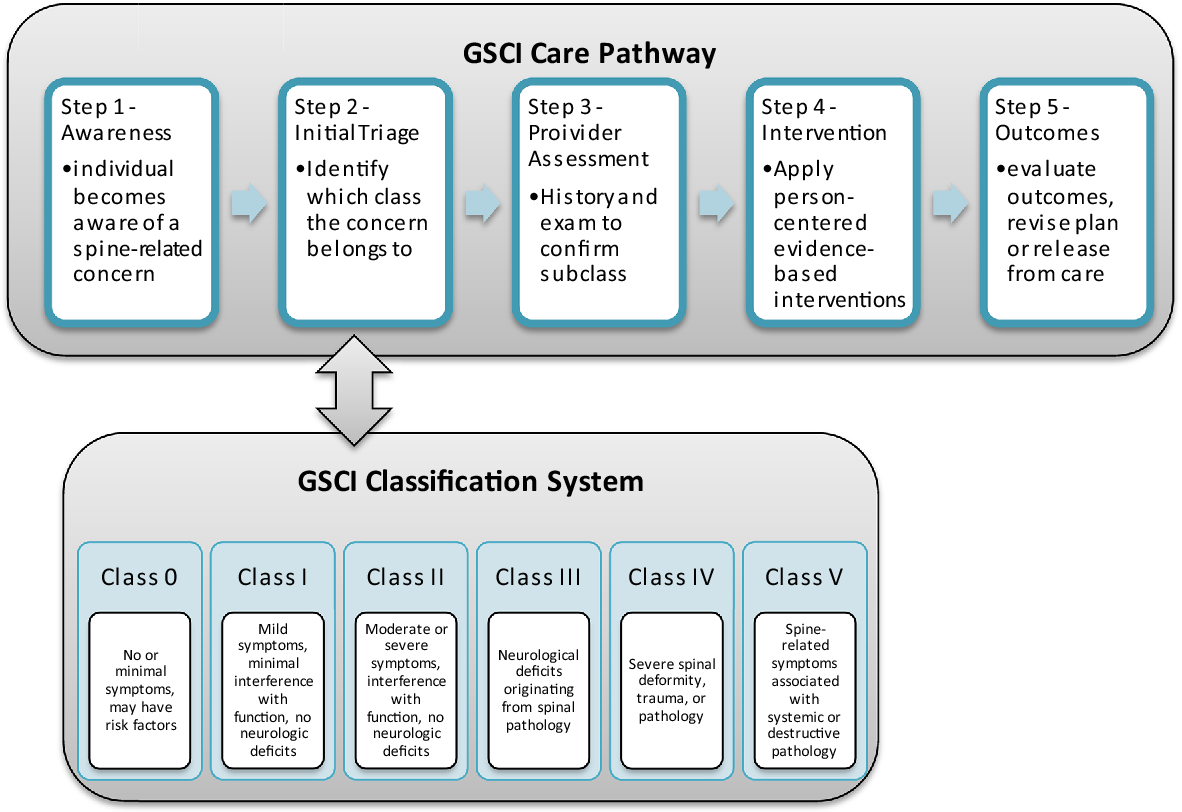
OBJECTIVE: Chiropractors and osteopaths are important professional partners in the management of axial spondyloarthritis (axSpA). In view of recent advances in diagnosis and treatment, we sought to understand their current knowledge and working practices.
METHODS: A Web-based survey was advertised to chiropractors and osteopaths via the Royal College of Chiropractors and the Institute of Osteopathy.
RESULTS: Of 382 completed responses [237 chiropractors (62%) and 145 osteopaths (38%)], all were familiar with AS, but only 63 and 25% were familiar with the terms axSpA and non-radiographic axSpA, respectively. Seventy-seven per cent were confident with inflammatory back pain. Respondents routinely asked about IBD (91%), psoriasis (81%), acute anterior uveitis (49%), peripheral arthritis (71%), genitourinary/gut infection (56%), enthesitis (30%) and dactylitis (20%). Eighty-seven per cent were aware of the association between axSpA and HLA-B27. Only 29% recognized that axSpA was common in women. Forty per cent recommend an X-ray (pelvic in 80%) and, if normal, 27% would recommend MRI of the sacroiliac joints and whole spine. Forty-four per cent were aware of biologic therapies. Forty-three per cent were confident with the process of onward referral to rheumatology via the general practitioner (GP). The principal perceived barrier to onward referral was reluctance by the GP to accept their professional opinion.
There are more articles like this @ our: