The Global Spine Care Initiative: Applying Evidence-based Guidelines on the Non-invasive Management of Back and Neck Pain to Low- and Middle-income Communities
SOURCE: European Spine Journal 2018 (Sep); 27 (Suppl 6): 851–860
Roger Chou, Pierre Côté, Kristi Randhawa, Paola Torres, Hainan Yu, Margareta Nordin, Eric L. Hurwitz, Scott Haldeman, Christine Cedraschi
Department of Medical Informatics and Clinical Epidemiology,
Oregon Health and Science University,
Portland, OR, USA.
PURPOSE: The purpose of this review was to develop recommendations for the management of spinal disorders in low-income communities, with a focus on non-invasive pharmacological and non-pharmacological therapies for non-specific low back and neck pain.
METHODS: We synthesized two evidence-based clinical practice guidelines for the management of low back and neck pain. Our recommendations considered benefits, harms, quality of evidence, and costs, with attention to feasibility in medically underserved areas and low- and middle-income countries.
RESULTS: Clinicians should provide education and reassurance, advise patients to remain active, and provide information about self-care options. For acute low back and neck pain without serious pathology, primary conservative treatment options are exercise, manual therapy, superficial heat, and nonsteroidal anti-inflammatory drugs (NSAIDs).
There are more articles like this @ our:
LOW BACK PAIN Page and the:
For patients with chronic low back and neck pain without serious pathology, primary treatment options are exercise, yoga, cognitive behavioral therapies, acupuncture, biofeedback, progressive relaxation, massage, manual therapy, interdisciplinary rehabilitation, NSAIDs, acetaminophen, and antidepressants. For patients with spinal pain with radiculopathy, clinicians may consider exercise, spinal manipulation, or NSAIDs; use of other interventions requires extrapolation from evidence regarding effectiveness for non-radicular spinal pain. Clinicians should not offer treatments that are not effective, including benzodiazepines, botulinum toxin injection, systemic corticosteroids, cervical collar, electrical muscle stimulation, short-wave diathermy, transcutaneous electrical nerve stimulation, and traction.
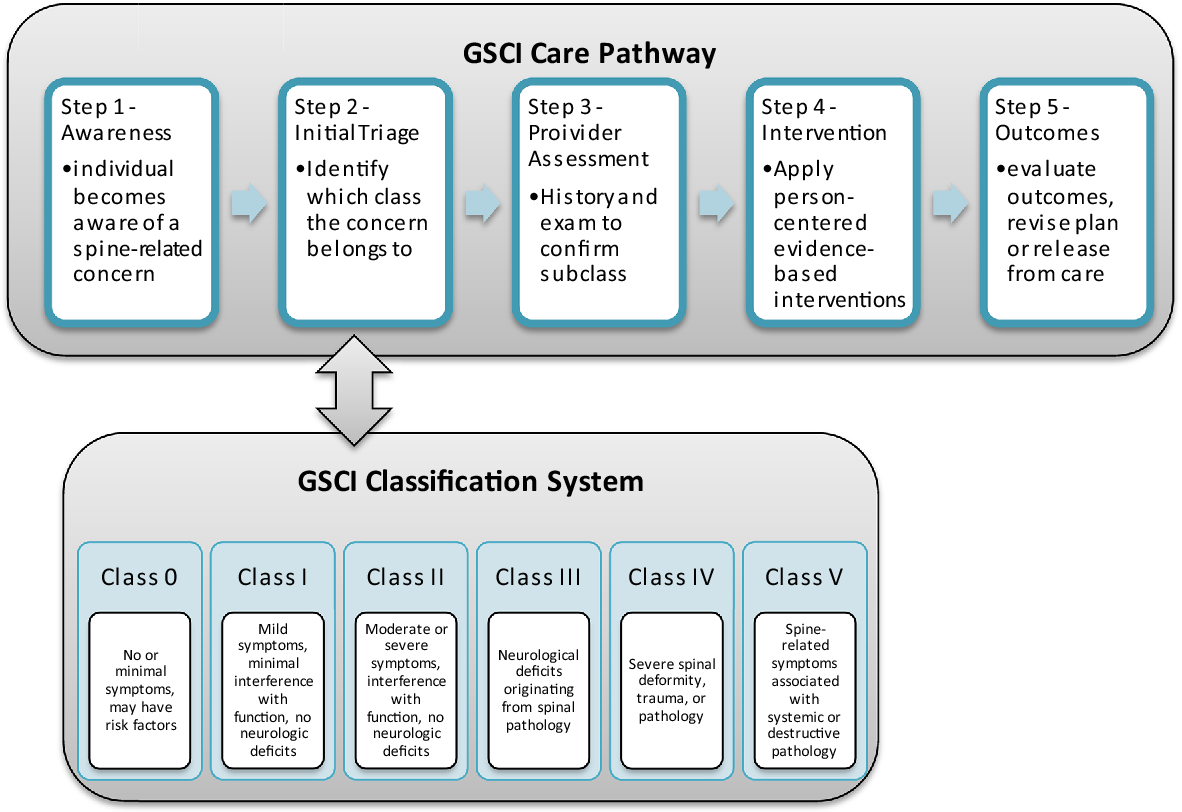
CONCLUSION: Guidelines developed for high-income settings were adapted to inform a care pathway and model of care for medically underserved areas and low- and middle-income countries by considering factors such as costs and feasibility, in addition to benefits, harms, and the quality of underlying evidence. The selection of recommended conservative treatments must be finalized through discussion with the involved community and based on a biopsychosocial approach. Decision determinants for selecting recommended treatments include costs, availability of interventions, and cultural and patient preferences. These slides can be retrieved under Electronic Supplementary Material.
KEYWORDS: Conservative treatment; Low back pain; Medically underserved area; Neck pain; Spine; Therapeutics
From the FULL TEXT Article:
Introduction
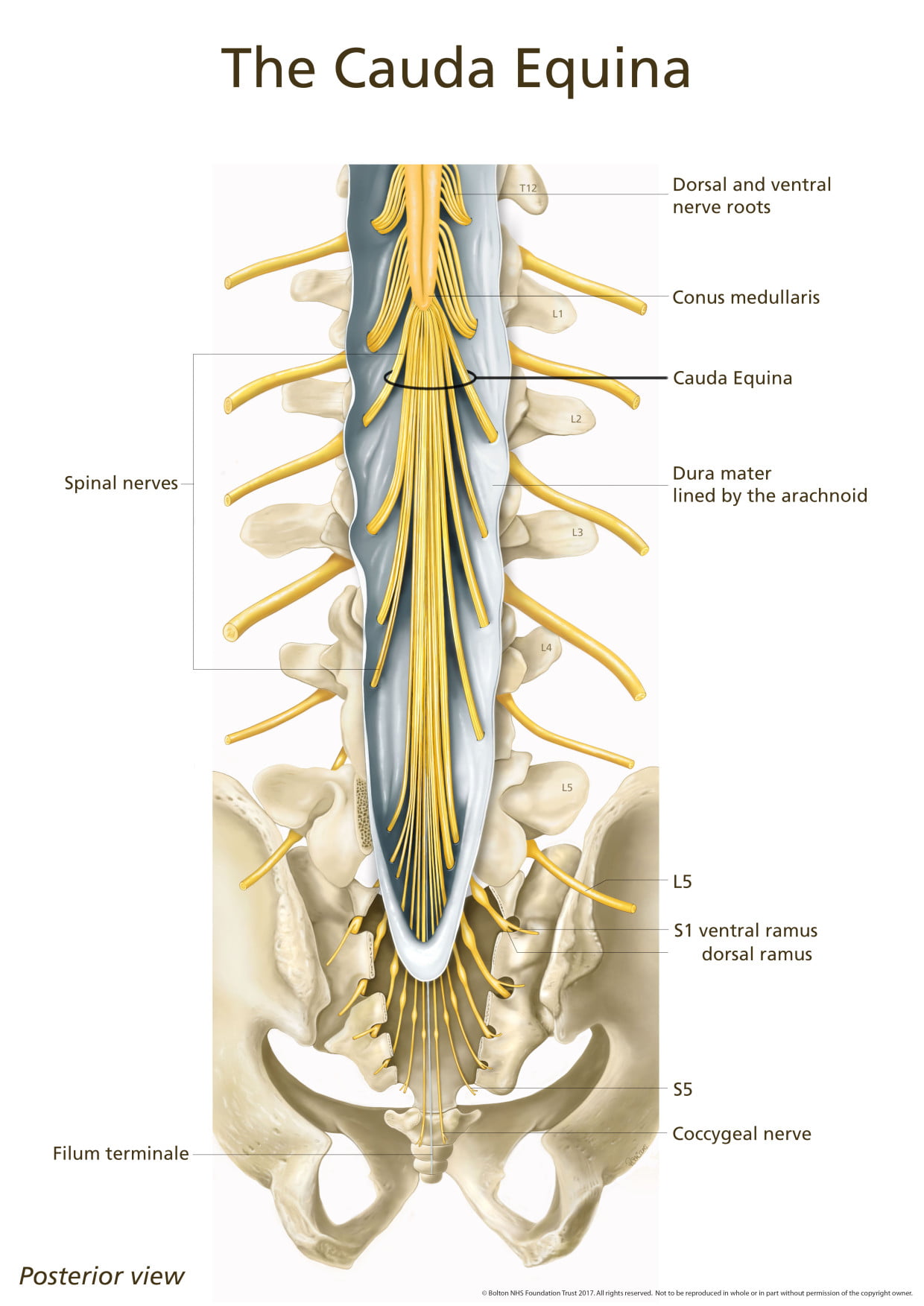
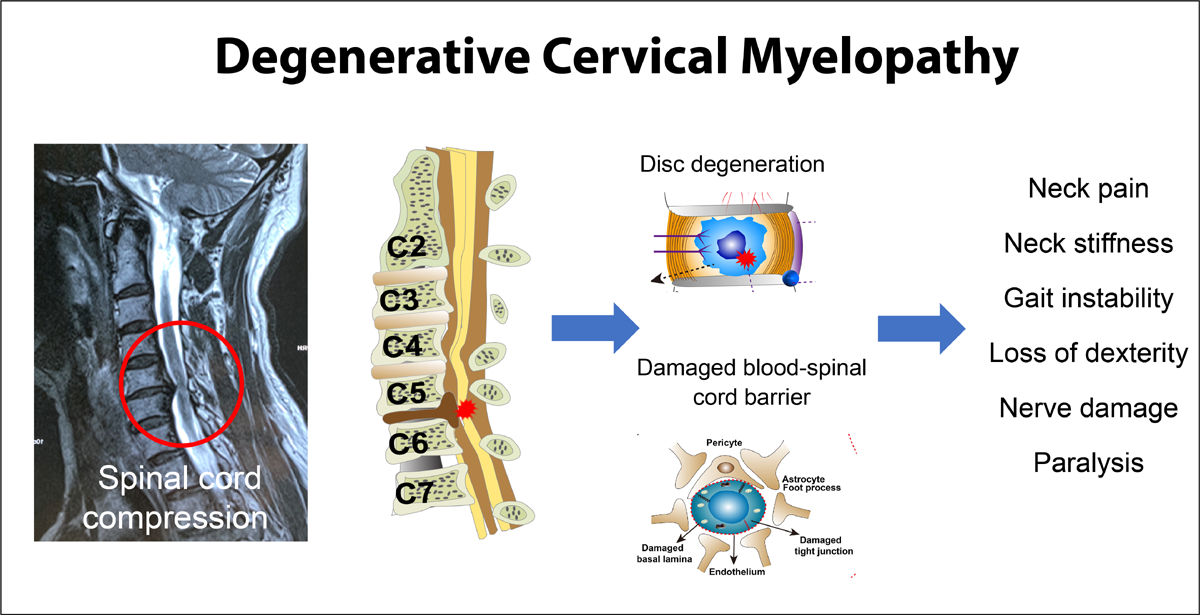
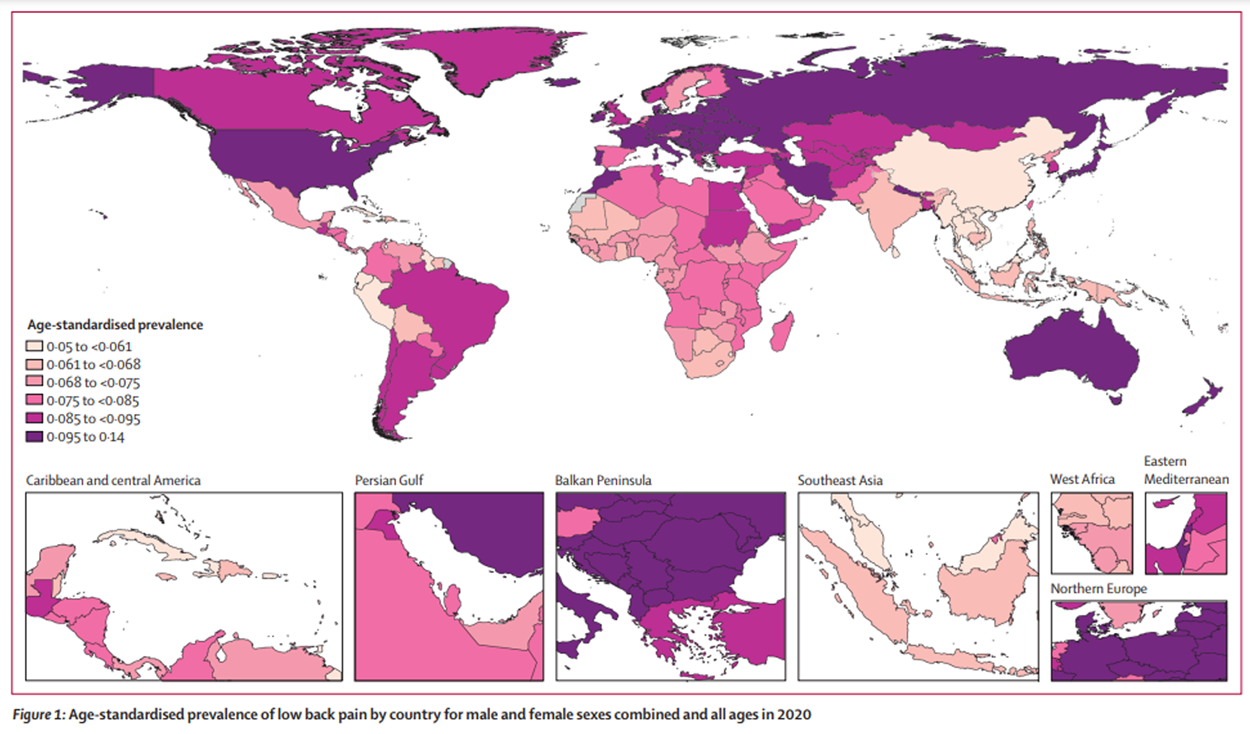
Spinal disorders are common worldwide. [1] They are a major contributor to the global disability burden and result in significant costs to health care and social security systems. [1, 2] The most common spinal disorders are nonspecific back and neck pain, which affect approximately one billion adults worldwide. [1] It is estimated that 8.9 and 4.8% of the world’s population, respectively, experienced low back pain (LBP) and neck pain, for longer than 3 months in 2013. [1] More importantly, low back and neck pain are the first and fourth most common disabling conditions worldwide. [1] Most spinal disorders are non-specific in that they cannot be reliably attributed to a specific underlying condition such as cancer, infection, ankylosing spondylitis, or other inflammatory or infectious diseases. [3] Although degenerative changes may be seen in patients with non-specific spinal disorders, such findings are common and age-related and their presence only weakly correlates with the presence and severity of symptoms. Only 1–2% of individuals with spinal pain have a serious pathology (e.g., cancer, infection, cauda equina syndrome). [4, 5] The prevalence of radicular LBP is about 12% or less, most commonly caused by disc herniation. [6, 7]
Evidence-based clinical practice guidelines are available to assist clinicians with the management of neck and LBP. These guidelines recommend that clinicians reassure patients that the prognosis of non-specific back and neck pain is favorable and advise patients to remain active. [8–10] First line pharmacologic options include nonsteroidal antiinflammatory drugs (NSAIDs) and acetaminophen, and recommended non-pharmacologic options include education, psychological interventions, exercise, spinal manipulation, and other complementary and alternative therapies. [11–14] The purpose of these interventions is to reduce pain, improve function, and address psychological contributors to pain. Prior guidelines have generally been developed based on literature conducted in high-income countries and for use in such settings. Feasibility and implementation in low- and middle income communities were not considered in prior guideline development efforts. [15]
The purpose of this article was to develop recommendations to the Global Spine Care Initiative care pathway and model of care for the management of non-specific low back and neck pain with a focus on non-invasive pharmacological and non-pharmacological therapies in medically underserved areas and low- and middle-income countries.
Read the rest of this Full Text article now!


Leave A Comment