New WHO Guideline on Chronic LBP: Global Impact
New WHO Guideline on Chronic LBP: Global Impact
World Health Organization Guideline:
Yes to Chiropractic; No to Most Drugs
SOURCE: Dynamic Chiropractic ~ February 2024
WHAT YOU NEED TO KNOW
|
On Dec. 7, 2023, the World Health Organization (WHO) released its “Guideline for Non-Surgical Management of Chronic Primary Low Back Pain in Adults in Primary and Community Care Settings.” [1] The purpose of the 244-page document is to “provide evidence-based recommendations on nonsurgical interventions for chronic primary LBP in adults” that will improve outcomes. “Spinal manipulative therapy” which includes chiropractic, is among the interventions the guideline recommends for all adults, including older adults.
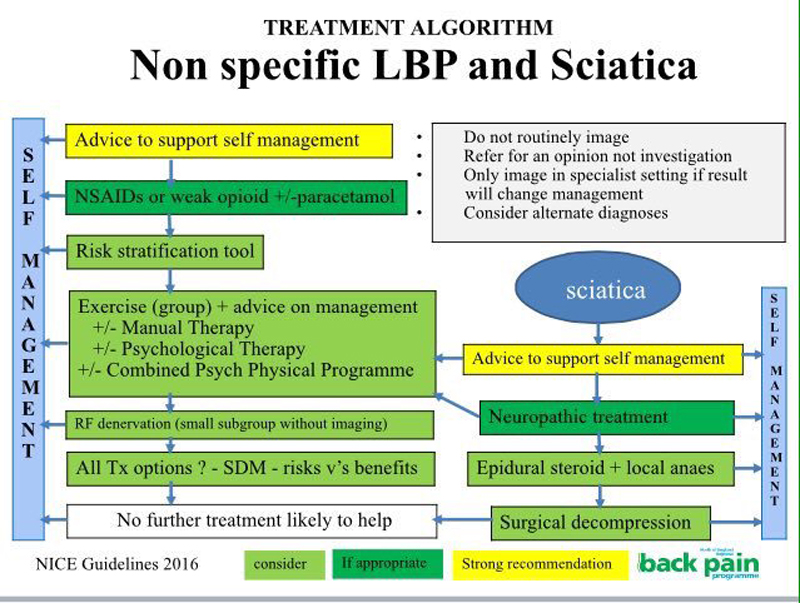
The guideline reviews both the benefits and the harms of nonsurgical interventions in the management of chronic primary LBP. In addition to spinal manipulative therapy, the guideline is also in favor of structured exercise, acupuncture, massage, NSAIDs and topical cayenne pepper (Capsicum frutescens).
NSAIDs continue to be the only recommended pharmacotherapy. Among the medication interventions the guideline recommends against are opioids, antidepressants (tricyclic, serotonin and noradrenaline reuptake inhibitor), skeletal muscle relaxants, injectable local anaesthetics and pharmacological weight-loss medications.
Acetaminophen, benzodiazepines and cannabis-related pharmaceutical preparations received “no recommendation,” while listing potential harmful effects including “cardiovascular, renal and gastrointestinal harms and increased mortality risk” for acetaminophen; “potential harms including memory impairment, misuse, overdose deaths from respiratory depression, somnolence, fatigue and light-headedness potentially leading to falls” for benzodiazepines; and “evidence of possible adverse events, including harms associated with its nonmedicinal use” for cannabis-related pharmaceutical preparations.
There are more articles like this @