National Clinical Guidelines for Non-surgical Treatment of Patients with Recent Onset Low Back Pain or Lumbar Radiculopathy
SOURCE: European Spine Journal 2018 (Jan); 27 (1): 60–75
Mette Jensen Stochkendahl, Per Kjaer,
Jan Hartvigsen, Alice Kongsted1,
Jens Aaboe, Margrethe Andersen, et al.
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmark,
Campusvej 55, 5230, Odense M, Denmark.
PURPOSE: To summarise recommendations about 20 non-surgical interventions for recent onset (<12 weeks) non-specific low back pain (LBP) and lumbar radiculopathy (LR) based on two guidelines from the Danish Health Authority.
This is just one article from a series of 5:
METHODS: Two multidisciplinary working groups formulated recommendations based on the GRADE approach.
RESULTS: Sixteen recommendations were based on evidence, and four on consensus. Management of LBP and LR should include information about prognosis, warning signs, and advise to remain active. If treatment is needed, the guidelines suggest using patient education, different types of supervised exercise, and manual therapy. The guidelines recommend against acupuncture, routine use of imaging, targeted treatment, extraforaminal glucocorticoid injection, paracetamol, NSAIDs, and opioids.
There are more articles like this @ our:
Low Back Pain and Chiropractic Page and the:
CONCLUSION: Recommendations are based on low to moderate quality evidence or on consensus, but are well aligned with recommendations from international guidelines. The guideline working groups recommend that research efforts in relation to all aspects of management of non-specific low back pain (LBP) and lumbar radiculopathy (LR) be intensified.
KEYWORDS: Clinical guideline; Conservative treatment; Low back pain; Lumbar radiculopathy; Non-surgical intervention; Recommendations
From the FULL TEXT Article:
Background
In 2012, the Danish Finance Act appropriated a total of €10.8 mio for the preparation of clinical guidelines. The Danish Health Authority (DHA) was subsequently commissioned to formulate 47 national clinical guidelines to support evidence-based decision making within health areas with a high burden of disease, a perceived large variation in practice, or uncertainty about which care was appropriate. [1] Two of these areas were low back pain (LBP) and lumbar radiculopathy (LR).
Consequently in 2014, two working groups were formed with the aim of developing national clinical guidelines for non-surgical interventions for recent onset (<12 weeks) LBP and for recent onset (<12 weeks) LR. The primary target groups for these guidelines were primary sector healthcare providers, i.e., general practitioners, chiropractors, and physiotherapists, but also medical specialists or others in the primary or secondary healthcare sector handling patients with LBP or LR.
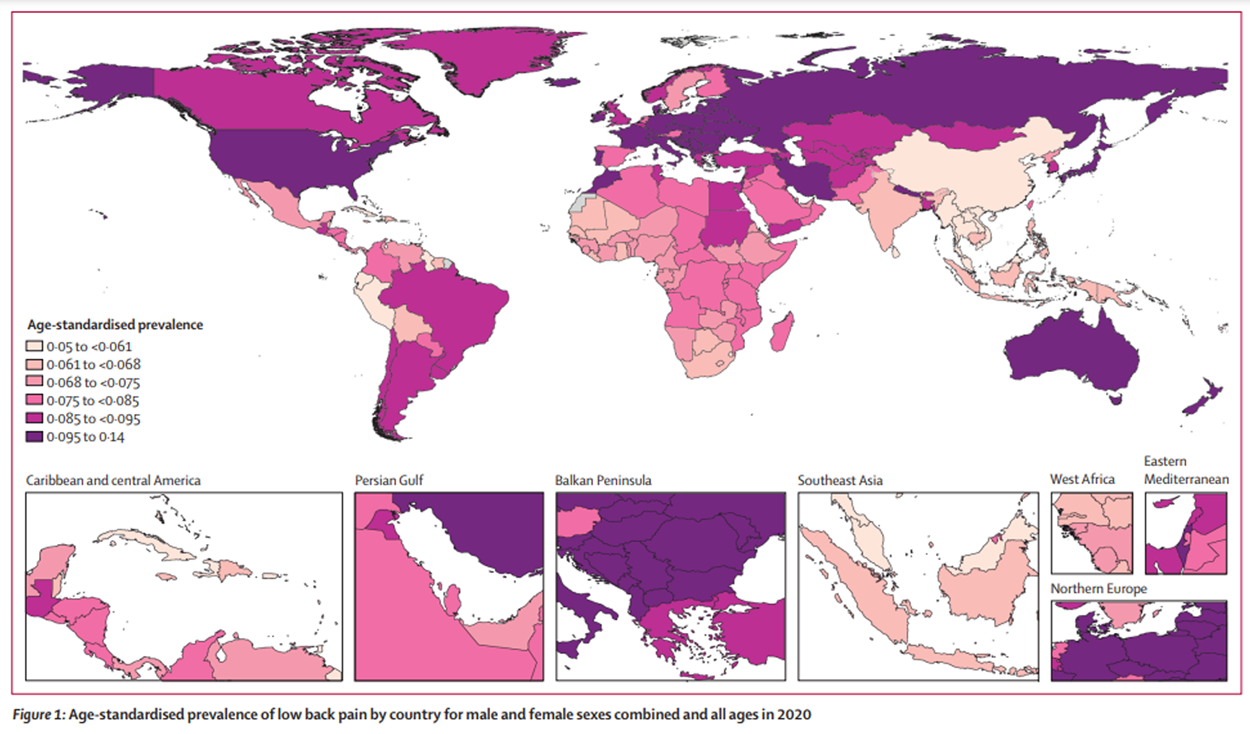
An estimated 15% of the Danish population suffers from low back pain (LBP) [2], and most will experience LBP during their lifetime [3], which is in accordance with estimates globally. [4] Both globally [5] and in Denmark [6], LBP with or without LR is a leading cause of years lived with disability, and consequently has major socioeconomic impact on society. For example, out of the 2.9 million Danes in the workforce, those with LBP have 5.5 million more days off work annually when compared to those without LBP, which accounts for 20% of all sick days, and LBP with or without LR is the most common reason for seeing a general practitioner, accounting for almost one in ten visits. [2]
In addition, Danes with LBP visit their general practitioner 3.3 times more often compared to Danes without LBP, and they consult approximately 30% more often chiropractors and physiotherapists. [2] Once you have had an episode of LBP, most will experience recurrences [7], and only a minority will stay pain free for longer periods of time. [8] Additionally, 1–10% of patients with LBP will experience LR, which is associated with a poorer prognosis compared to LBP without LR. [9]
This paper summarises the two Danish national clinical guidelines, which were published in 2016 as full reports in Danish. [10, 11] The mandates for the two working groups were to make recommendations based on a maximum of ten clinical questions for LBP and LR each. The working groups were not asked to make recommendations for diagnostic procedures or care pathways.
Read the rest of this Full Text article now!



Leave A Comment