Spinal Manipulative Therapy and Other Conservative Treatments for Low Back Pain:
A Guideline From the Canadian Chiropractic Guideline Initiative
SOURCE: J Manipulative Physiol Ther. 2018 (Mar 29) [Epub]
André E. Bussières, DC, FCCS(C), PhD, Gregory Stewart, DC, Fadi Al-Zoubi, PT, MSc, Philip Decina, DC, Martin Descarreaux, DC, PhD, Danielle Haskett, BSc, Cesar Hincapié, DC, PhD, Isabelle Pagé, DC, MSc, Steven Passmore, DC, PhD, John Srbely, DC, PhD, Maja Stupar, DC, PhD, Joel Weisberg, DC, Joseph Ornelas, DC, PhD
School of Physical and Occupational Therapy,
Faculty of Medicine, McGill University,
Montreal, Québec, Canada
OBJECTIVE:   The objective of this study was to develop a clinical practice guideline on the management of acute and chronic low back pain (LBP) in adults. The aim was to develop a guideline to provide best practice recommendations on the initial assessment and monitoring of people with low back pain and address the use of spinal manipulation therapy (SMT) compared with other commonly used conservative treatments.
METHODS:   The topic areas were chosen based on an Agency for Healthcare Research and Quality comparative effectiveness review, specific to spinal manipulation as a nonpharmacological intervention. The panel updated the search strategies in Medline. We assessed admissible systematic reviews and randomized controlled trials for each question using A Measurement Tool to Assess Systematic Reviews and Cochrane Back Review Group criteria. Evidence profiles were used to summarize judgments of the evidence quality and link recommendations to the supporting evidence. Using the Evidence to Decision Framework, the guideline panel determined the certainty of evidence and strength of the recommendations. Consensus was achieved using a modified Delphi technique. The guideline was peer reviewed by an 8-member multidisciplinary external committee.
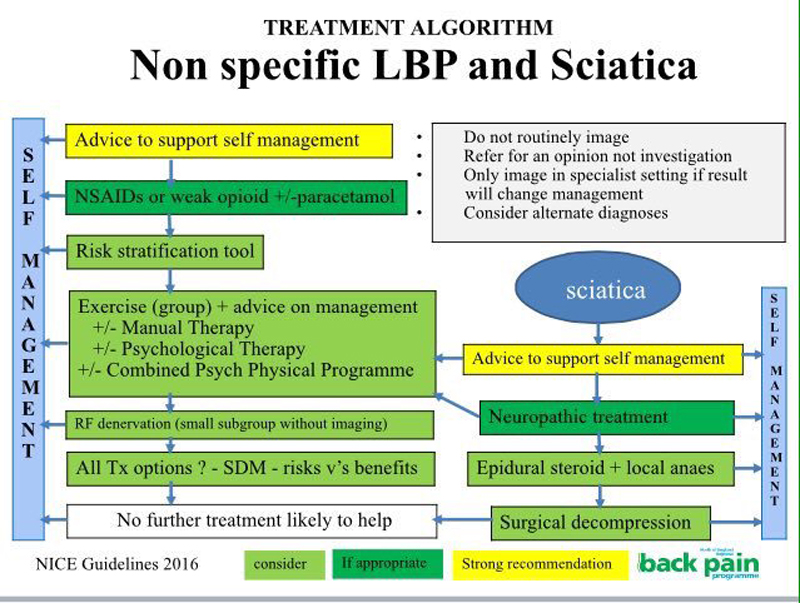
RESULTS:   For patients with acute (0-3 months) back pain, we suggest offering advice (posture, staying active), reassurance, education and self-management strategies in addition to SMT, usual medical care when deemed beneficial, or a combination of SMT and usual medical care to improve pain and disability. For patients with chronic (>3 months) back pain, we suggest offering advice and education, SMT or SMT as part of a multimodal therapy (exercise, myofascial therapy or usual medical care when deemed beneficial). For patients with chronic back-related leg pain, we suggest offering advice and education along with SMT and home exercise (positioning and stabilization exercises).
There are more articles like this @ our:
CONCLUSIONS:   A multimodal approach including SMT, other commonly used active interventions, self-management advice, and exercise is an effective treatment strategy for acute and chronic back pain, with or without leg pain.
KEYWORDS:   Chiropractic; Conservative Treatment; Disease Management; Low Back Pain; Practice Guideline
From the FULL TEXT Article:
Introduction
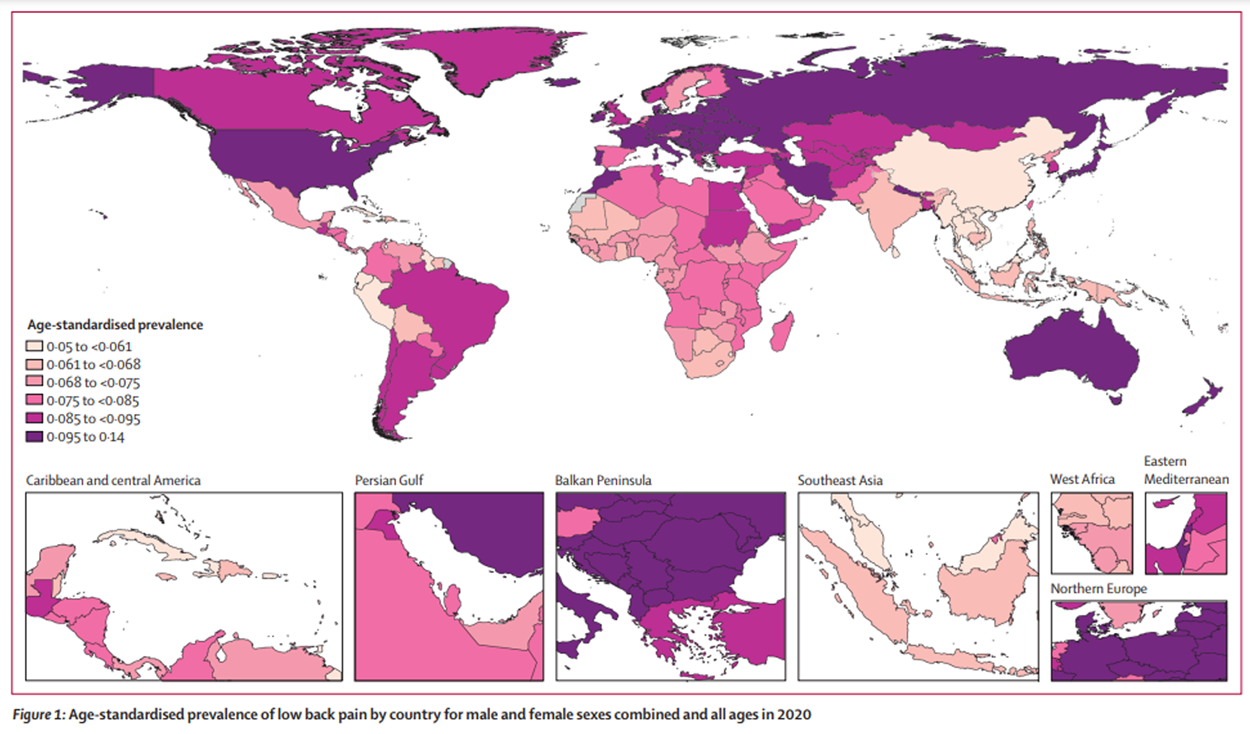
In 2015, musculoskeletal (MSK) disorders were the largest contributor to global years lived with disability (YLDs) (18.5% [16.4%-20.9%] of all YLDs). [1] Approximately half (49.6%) of the YLDs stem from low back pain (LBP). [1, 2] The point prevalence of LBP is estimated at nearly 20%, the 1–year prevalence is around 50%, and the lifetime prevalence is about 85% in the general population. [3] Despite the availability of many clinical interventions to manage LBP, [4] a nearly 3–fold increase in the prevalence of chronic LBP was observed between 1992 (3.9%, 95% confidence interval [CI] 3.4%-4.4%) and 2006 (10.2%, 95% CI 9.3%-11.0%). [5]
Affecting more than 630 million people worldwide, [6] LBP results in significant physical, psychological, and social burden and high cost to society. [7] People with LBP tend to experience a higher proportion of functional disability, dysfunctional family relationships, depression, social isolation, work absence, and poor work productivity. [8–14] They have a lower socioeconomic status and a lower quality of life, but tend to be higher users of health care services. [8, 11, 15] Chronic LBP is associated with significant comorbidities, including diabetes, coronary heart disease, [16–18] and depression. [19] The economic burden of LBP is significant. [7, 20, 21] In the United States, the direct and indirect costs of LBP are estimated to exceed 100 billion dollars per year. [5, 22] In Canada, the LBP-related estimate of the medical costs ranges between 6 and 12 billion dollars annually. [23]
Read the rest of this Full Text article now!



Leave A Comment