The Effect of Reduced Access to Chiropractic Care on Medical Service Use for Spine Conditions Among Older Adults
The Effect of Reduced Access to Chiropractic Care on Medical Service Use for Spine Conditions Among Older Adults
SOURCE: J Manipulative Physiol Ther 2021 (Aug 7)
Matthew Davis, Olga Yakusheva, Haiyin Liu, Brian Anderson, Julie Bynum
University of Michigan,
400 North Ingalls, Room 4347,
Ann Arbor, MI 48109
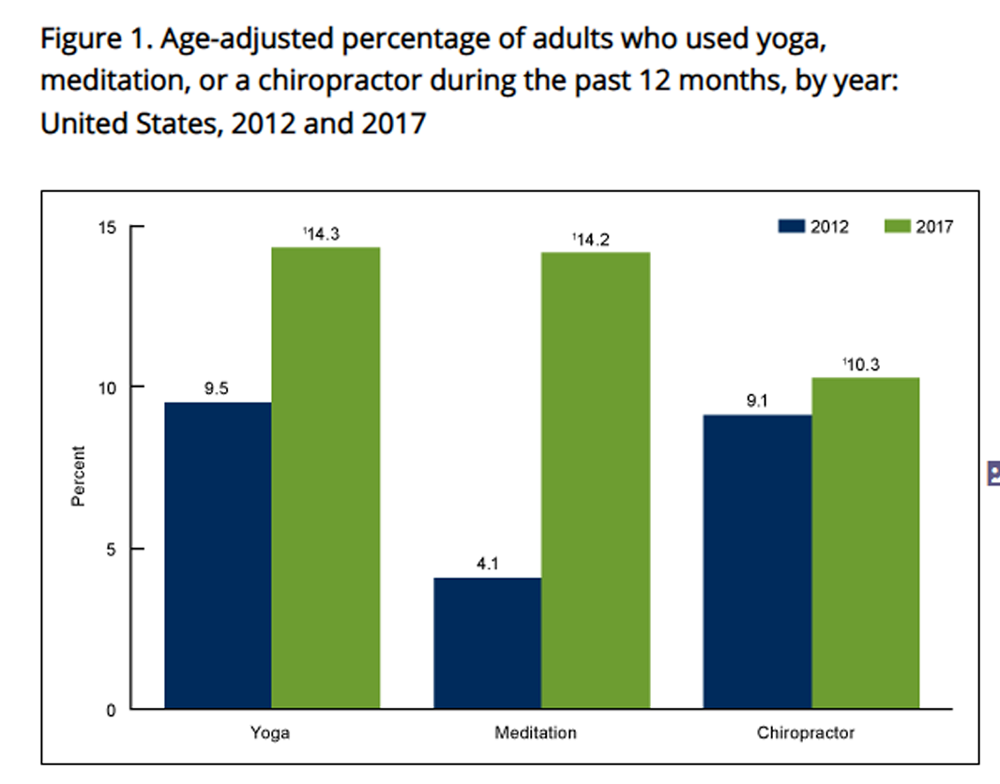
Objective: The purpose of this study was to examine the extent to which access to chiropractic care affects medical service use among older adults with spine conditions.
Methods: We used Medicare claims data to identify a cohort of 39,278 older adult chiropractic care users who relocated during 2010-2014 and thus experienced a change in geographic access to chiropractic care. National Plan and Provider Enumeration System data were used to determine chiropractor per population ratios across the United States. A reduction in access to chiropractic care was defined as decreasing 1 quintile or more in chiropractor per population ratio after relocation. Using a difference-in-difference analysis (before versus after relocation), we compared the use of medical services among those who experienced a reduction in access to chiropractic care versus those who did not.
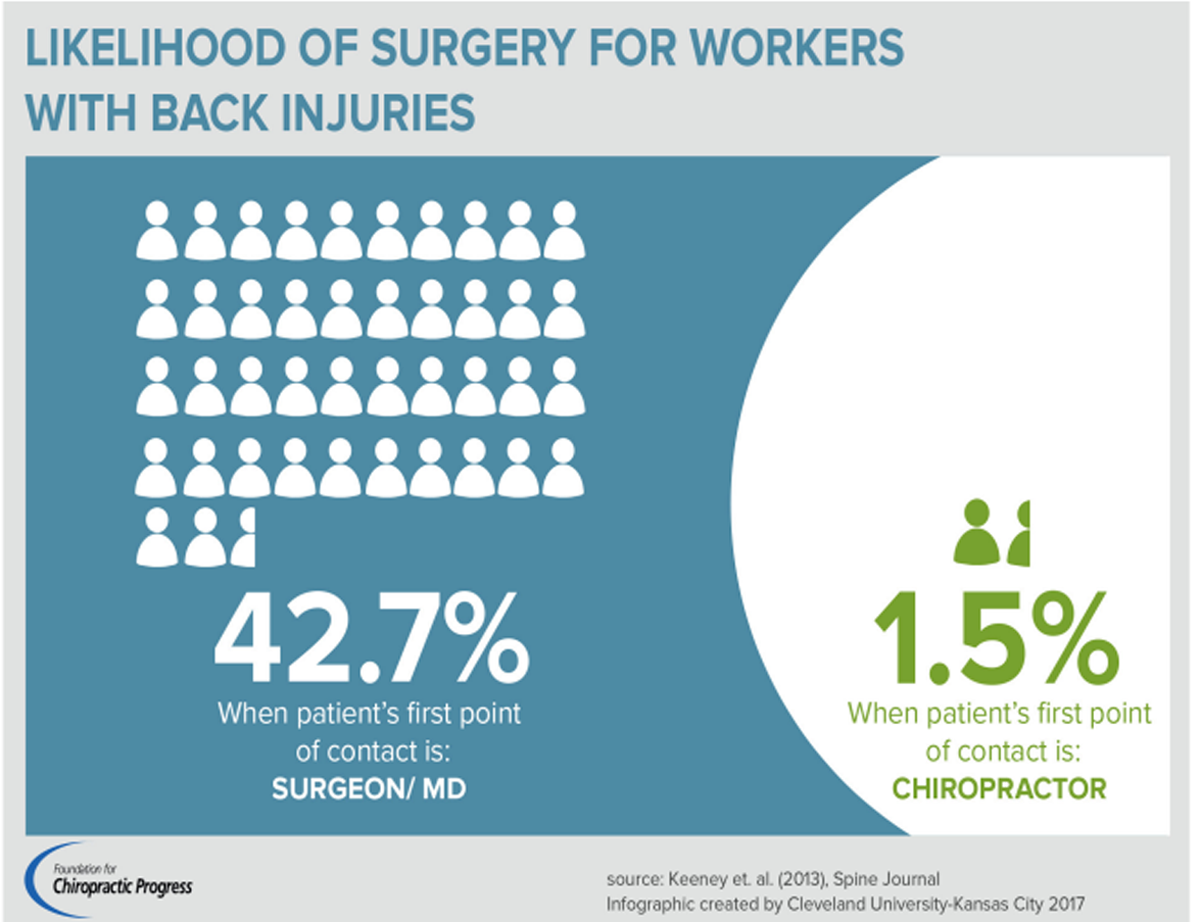
Results: Among those who experienced a reduction in access to chiropractic care (versus those who did not), we observed an increase in the rate of visits to primary care physicians for spine conditions (an annual increase of 32.3 visits, 95% CI: 1.4-63.1 per 1,000) and rate of spine surgeries (an annual increase of 5.5 surgeries, 95% CI: 1.3-9.8 per 1,000). Considering the mean cost of a visit to a primary care physician and spine surgery, a reduction in access to chiropractic care was associated with an additional cost of $114,967 per 1,000 beneficiaries on medical services ($391 million nationally).
There are more articles like this @ our: