The Vast Majority of Patients With Fibromyalgia Have a Straight Neck Observed on a Lateral View Radiograph of the Cervical Spine: An Aid in the Diagnosis of Fibromyalgia and a Possible Clue to the Etiology
The Vast Majority of Patients With Fibromyalgia Have a Straight Neck Observed on a Lateral View Radiograph of the Cervical Spine: An Aid in the Diagnosis of Fibromyalgia and a Possible Clue to the Etiology
SOURCE: J Clinical Rheumatology 2022 (Nov 3) [EPUB]
| OPEN ACCESS |
Robert S Katz, MD, Frank Leavitt, PhD, Katya Cherny,MS , Alexandra Katz Small, MD, Ben J Small, MD
From the Rush Medical University.
Rheumatology Associates.
Northwestern University Medical Center,
Chicago, IL.
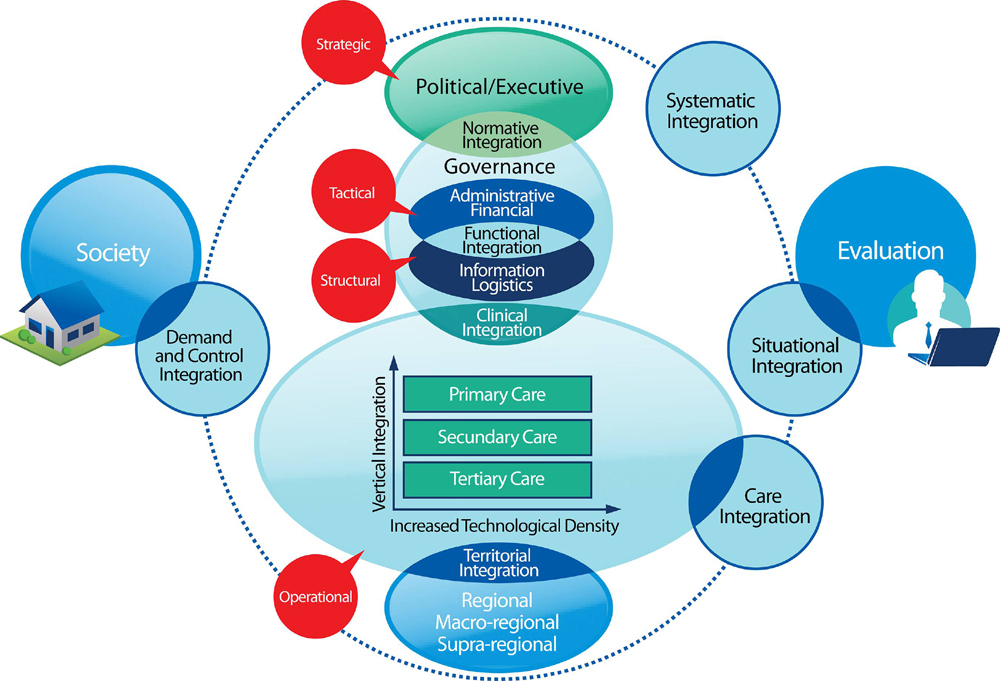
Objective: A straight cervical spine is an underappreciated and often overlooked finding in fibromyalgia. The aim of this medical records review study was to evaluate the cervical curvature on radiographs of patients with fibromyalgia.
Methods: A consecutive series of 270 cervical spine radiographs of patients with neck pain from 2015 to 2018 were retrospectively analyzed for cervical curvature using the Cobb angle measurement. One hundred fifty-five patients met full American College of Rheumatology criteria for fibromyalgia, whereas 115 subjects with other rheumatic diseases who were similar in age and education served as control subjects.
Results: Mean cervical curvature in fibromyalgia was 6.4 ± 5.2 degrees and 13.8 ± 7.4 degrees in control subjects. The more than 7-degree difference was significant (p < 0.001). Curvature in the magnitude of 21 degrees is at the low end of normal. At ≤10 degrees, where the cervical spine is essentially straight, there were 129 fibromyalgia patients (83.2%) and 37 control subjects (32.2%). The 51% difference was significant (p < 0.001).
There is more like this @ our:RADIOLOGY Section and the:
FIBROMYALGIA Section and the: