Patient-reported Improvements of Pain, Disability, and Health-related Quality of Life Following Chiropractic Care for Back Pain
Patient-reported Improvements of Pain, Disability, and Health-related Quality of Life Following Chiropractic Care for Back Pain – A National Observational Study in Sweden
SOURCE: J Bodyw Mov Ther. 2019 (Apr); 23 (2): 241–246
Gedin F, MSc; Dansk V, MSc; Egmar A-C, PhD; Sundberg T, PhD; Burström K, PhD
Health Economics and Economic Evaluation Research Group,
Medical Management Centre,
Karolinska Institutet,
Stockholm, Sweden
BACKGROUND: Chiropractic care is a common but not often investigated treatment option for back pain in Sweden. The aim of this study was to explore patient-reported outcomes (PRO) for patients with back pain seeking chiropractic care in Sweden.
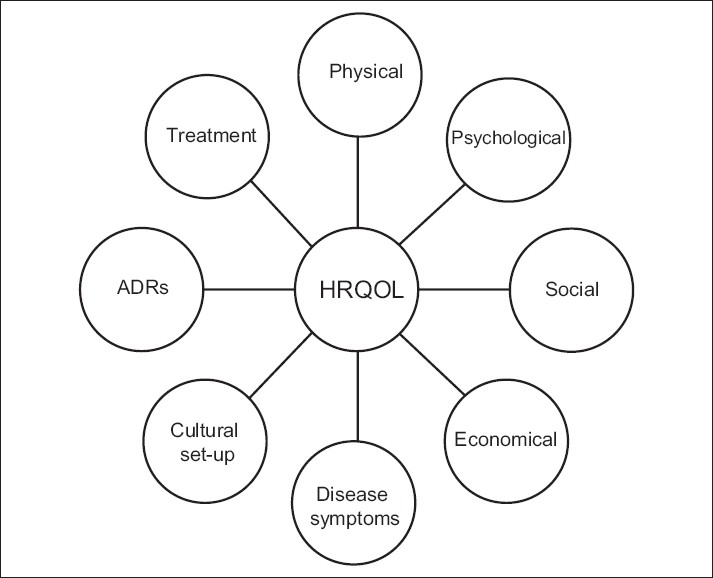
METHODS: Prospective observational study. Patients 18 years and older, with non-specific back pain of any duration, seeking care at 23 chiropractic clinics throughout Sweden were invited to answer PRO questionnaires at baseline with the main follow-up after four weeks targeting the following outcomes: Numerical Rating Scale for back pain intensity (NRS), Oswestry Disability Index for back pain disability (ODI), health-related quality of life (EQ-5D index) and a visual analogue scale for self-rated health (EQ VAS).
There are more articles like this @ our: