Different Placebos, Different Mechanisms, Different Outcomes: Lessons for Clinical Trials
SOURCE: PLoS One. 2015 (Nov 4); 10 (11): e0140967
Fabrizio Benedetti, and Sara Dogue
University of Turin Medical School,
Neuroscience Department,
Turin, Italy.
|
I have been fascinated with placebo-controlled trials since the 90s. In those days, virtually all the placebo-controlled manipulative trials claimed that SMT was *no better than placebo*. And in those days, medicine looked down their long noses, considering placebo as worthless, a mild side-effect of trickery and quackery. “A patient finally went to a chiropractor for her back pain after finding no relief with the orthopedist. After three adjustments and a week of no symptoms, she had a follow-up visit with her M.D. Upon learning about the success of the D.C., the orthopedist stated, “That was just the placebo effect.” The patient responded, “If it works so well, why didn’t you use it?” –– Attributed to Robert Mootz, D.C.
Finally, I got around to copying several of those early SMT/placebo studies, and was pleasantly shocked to discover that, compared to pre-study findings, BOTH groups improved significantly. This did NOT mean SMT didn’t help patients, it just means that it didn’t help them MORE than the placebo did. It also strongly suggested that the plazcebo(s) were probably NOT inert. At any rate, now you know why I started collecrting articles on placebo, and they eventually coalesced (2002) into our topical Problem with Placebos/Shams Page. This is how many of our other Topical pages evolved from their humble beginnings. |
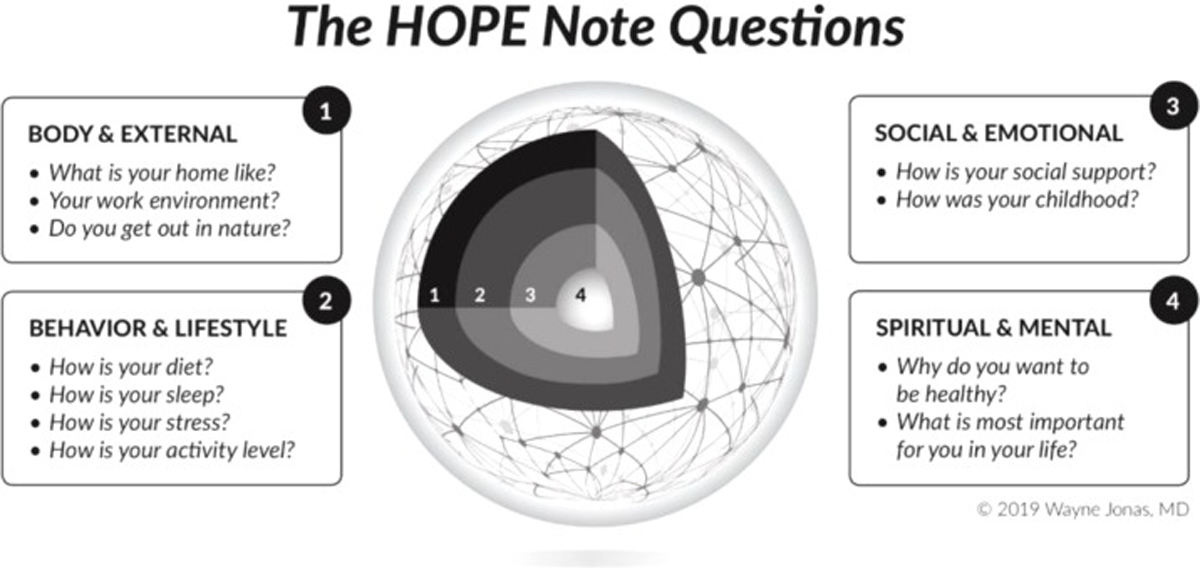
Clinical trials use placebos with the assumption that they are inert, thus all placebos are considered to be equal. Here we show that this assumption is wrong and that different placebo procedures are associated to different therapeutic rituals which, in turn, trigger different mechanisms and produce different therapeutic outcomes. We studied high altitude, or hypobaric hypoxia, headache, in which two different placebos were administered. The first was placebo oxygen inhaled through a mask, whereas the second was placebo aspirin swallowed with a pill.
There are more articles like this @ our:
Both placebos were given after a conditioning procedure, whereby either real oxygen or real aspirin was administered for three consecutive sessions to reduce headache pain. We found that after real oxygen conditioning, placebo oxygen induced pain relief along with a reduction in ventilation, blood alkalosis and salivary prostaglandin (PG)E2, yet without any increase in blood oxygen saturation (SO2). By contrast, after real aspirin conditioning, placebo aspirin induced pain relief through the inhibition of all the products of cyclooxygenase, that is, PGD2, PGE2, PGF2, PGI2, thromboxane (TX)A2, without affecting ventilation and blood alkalosis. Therefore, two different placebos, associated to two different therapeutic rituals, used two different pathways to reduce headache pain.
The analgesic effect following placebo oxygen was superior to placebo aspirin. These findings show that different placebos may use different mechanisms to reduce high altitude headache, depending on the therapeutic ritual and the route of administration. In clinical trials, placebos and outcome measures should be selected very carefully in order not to incur in wrong interpretations.
From the FULL TEXT Article:
Introduction
The use of placebo control groups is crucial in the current methodology of clinical trials. However, whereas a placebo is usually defined as an inert treatment devoid of any intrinsic therapeutic property, there is today some evidence that all placebos are not equal, some of them being more effective than others, for example in migraine [2] and osteoarthritis. [2] The differences across different placebos, e.g. oral, subcutaneous, topical, intra-articular placebos, as well as sham acupuncture needles, indicate that placebos are not inert but rather they are made of many psychosocial elements that build up the ritual of the therapeutic act. [3–5]
Recently, high altitude, or hypobaric hypoxia, headache has emerged as an interesting model to better understand the biological underpinnings of placebo analgesia. [6, 7] This kind of headache is part of a clinical condition known as acute mountain sickness (AMS), which is usually diagnosed by means of the Lake Louise Score (LLS) questionnaire. [8] This is aimed at detecting several symptoms, such as headache, nausea/vomiting, dizziness, insomnia, as well as neurological symptoms, which emphasize the complex nature of this hypoxia-related clinical syndrome. AMS is triggered by the drop in atmospheric oxygen pressure at high altitude. [9, 10]
Read the rest of this Full Text article now!




Leave A Comment