Pain-Related Fear-Dissociable Neural Sources
Pain-Related Fear-Dissociable Neural Sources of Different Fear Constructs
SOURCE: eNeuro. 2019 (Jan 3); 5 (6) pii: ENEURO.0107-18.2018
Michael Lukas Meier, Andrea Vrana, Barry Kim Humphreys, Erich Seifritz, Philipp Stämpfli, and Petra Schweinhardt
Integrative Spinal Research,
Department of Chiropractic Medicine,
Balgrist University Hospital,
8008 Zurich, Switzerland.
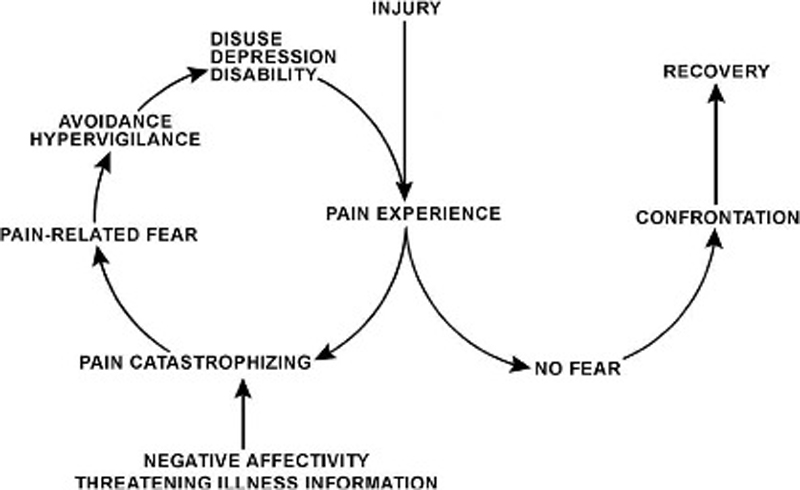
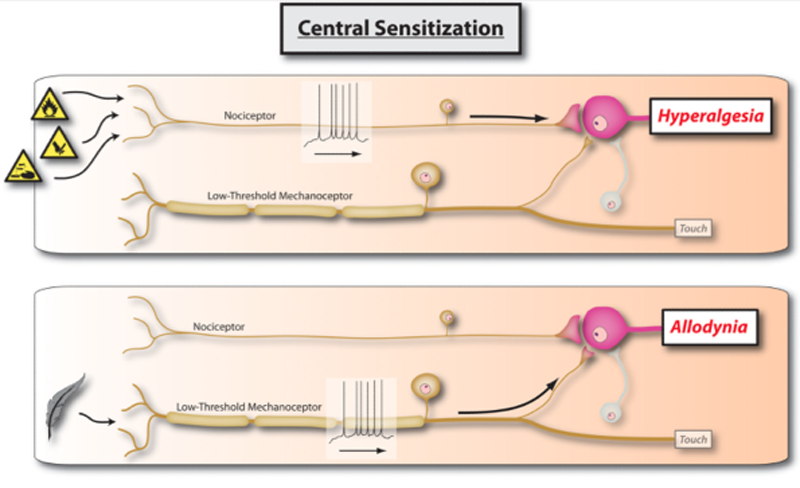
Fear of pain demonstrates significant prognostic value regarding the development of persistent musculoskeletal pain and disability. Its assessment often relies on self-report measures of pain-related fear by a variety of questionnaires. However, based either on “fear of movement/(re)injury/kinesiophobia,” “fear avoidance beliefs,” or “pain anxiety,” pain-related fear constructs plausibly differ while it is unclear how specific the questionnaires are in assessing these different constructs. Furthermore, the relationship of pain-related fear to other anxiety measures such as state or trait anxiety remains ambiguous. Advances in neuroimaging such as machine learning on brain activity patterns recorded by functional magnetic resonance imaging might help to dissect commonalities or differences across pain-related fear constructs. We applied a pattern regression approach in 20 human patients with nonspecific chronic low back pain to reveal predictive relationships between fear-related neural pattern information and different pain-related fear questionnaires.
More specifically, the applied multiple kernel learning approach allowed the generation of models to predict the questionnaire scores based on a hierarchical ranking of fear-related neural patterns induced by viewing videos of activities potentially harmful for the back. We sought to find evidence for or against overlapping pain-related fear constructs by comparing the questionnaire prediction models according to their predictive abilities and associated neural contributors. By demonstrating evidence of nonoverlapping neural predictors within fear-processing regions, the results underpin the diversity of pain-related fear constructs. This neuroscientific approach might ultimately help to further understand and dissect psychological pain-related fear constructs.
There are more articles like this @ our: