Evidence-Based Nonpharmacologic Strategies for Comprehensive Pain Care: The Consortium Pain Task Force White Paper
SOURCE: Explore (NY). 2018 (Mar 1) [Epub]
Heather Tick, MD, Arya Nielsen, PhD, Kenneth R. Pelletier, PhD, MD, Robert Bonakdar, MD, Samantha Simmons, MPH, Ronald Glick, MD, Emily Ratner, MD, Russell L. Lemmon, MD, Peter Wayne, PhD, Veronica Zador, BSc
Departments of Family Medicine,
Anesthesiology and Pain Medicine,
University of Washington School of Medicine,
Seattle, WA.
Medical pain management is in crisis; from the pervasiveness of pain to inadequate pain treatment, from the escalation of prescription opioids to an epidemic in addiction, diversion and overdose deaths. The rising costs of pain care and managing adverse effects of that care have prompted action from state and federal agencies including the
Department of Defense (DOD,
Veterans Health Administration (VHA),
National Institutes of Health (NIH),
Food and Drug Administration (FDA) and the
Centers for Disease Control and Prevention (CDC).
There is pressure for pain medicine to shift away from reliance on opioids, ineffective procedures and surgeries toward comprehensive pain management that includes evidence-based nonpharmacologic options. This White Paper details the historical context and magnitude of the current pain problem including individual, social and economic impacts as well as the challenges of pain management for patients and a healthcare workforce engaging prevalent strategies not entirely based in current evidence. Detailed here is the evidence-base for nonpharmacologic therapies effective in postsurgical pain with opioid sparing, acute non-surgical pain, cancer pain and chronic pain.
Therapies reviewed include
acupuncture therapy,
massage therapy,
osteopathic and chiropractic manipulation,
meditative movement therapies Tai chi and yoga,
mind body behavioral interventions,
dietary components and
self-care/self-efficacy strategies.
Transforming the system of pain care to a responsive comprehensive model necessitates that options for treatment and collaborative care must be evidence-based and include effective nonpharmacologic strategies that have the advantage of reduced risks of adverse events and addiction liability.
The evidence demands a call to action to increase awareness of effective nonpharmacologic treatments for pain, to train healthcare practitioners and administrators in the evidence base of effective nonpharmacologic practice, to advocate for policy initiatives that remedy system and reimbursement barriers to evidence-informed comprehensive pain care, and to promote ongoing research and dissemination of the role of effective nonpharmacologic treatments in pain, focused on the short- and long-term therapeutic and economic impact of comprehensive care practices.
There are more articles like this @ our:
Low Back Pain Page
and the:
KEYWORDS:   Chiropractic; Conservative Treatment; Disease Management; Low Back Pain; Practice Guideline
From the FULL TEXT Article:
SECTION 1: The Problem
Historical Context for a Call to Change
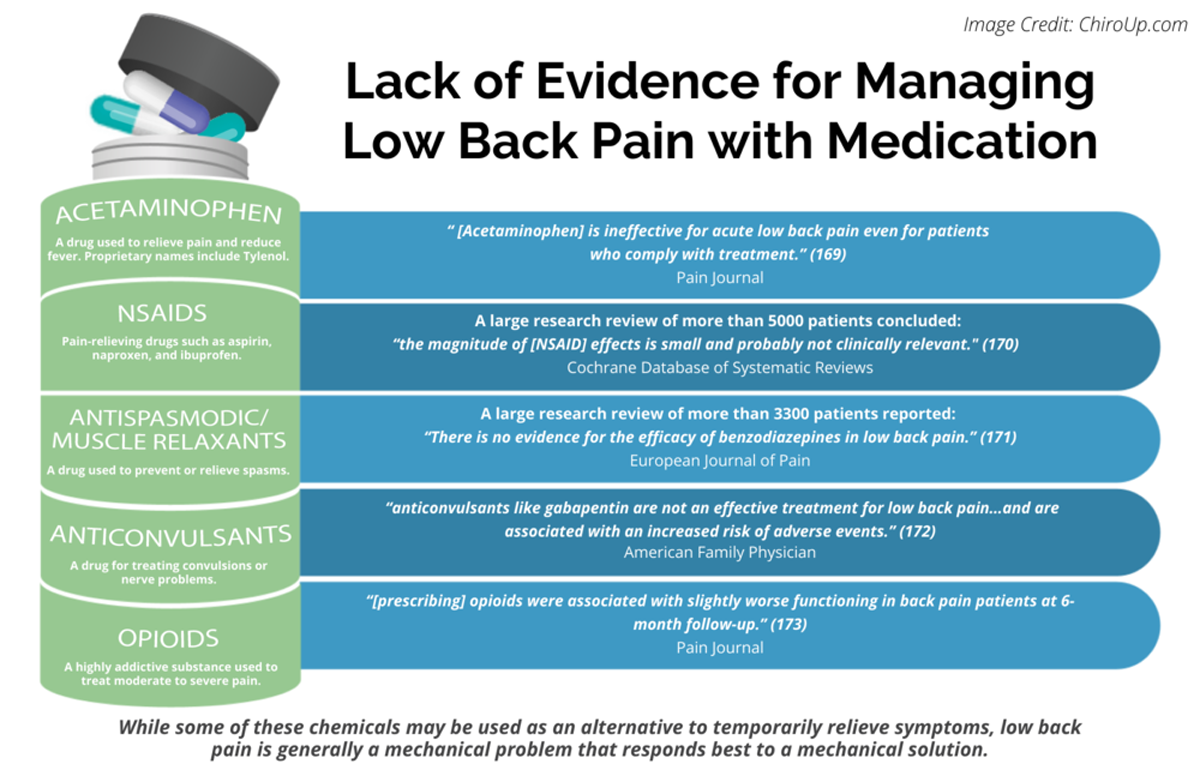
Pain care in America is in crisis. The prevalence of pain is high despite costly, well-intentioned medical responses, which rely mainly on pharmaceuticals and high-tech interventions. Pain and aspects of current pain management strategies are having enormous deleterious impacts on patients, the health system and society. [1, 2] From the 1970s to the 1990s there was hope that new drugs, more liberal use of opioids, new technologies and a growing understanding about the mechanisms of pain would reduce the occurrence of uncontrolled pain. This was not the case. Growing rates and escalating costs of pain-related morbidity, mortality and disability have led to calls for culture change in pain medicine by The Office of the Army Surgeon General Pain Management Task Force (PMTF) Report, [3] Institute of Medicine (IOM) (now the National Academy of Medicine, NAM), [1, 2] Interagency Pain Research Coordinating Committee’s National Pain Strategy [4] and others.
Government leaders have declared the opioid crisis a national emergency. The recommendations consistently promote a shift toward a more comprehensive, patient-centered and health-focused approach to pain patients. In this model, collaborative care is team-based, interdisciplinary, and involves both pharmacologic and nonpharmacologic approaches. The model affirms the essential role patients have in improving their own health and pain-related behaviors. There is a growing recognition that current conventional medical treatment may not be the best starting point and is often not sufficient. In addition to inadequately addressing pain there is increasing evidence that conventional treatment strategies are fueling the opioid crisis, according to a National Institute for Drug Abuse (NIDA) report citing one in three Americans used prescription opioids for pain in 2015. [5] Moreover, evidence-based nonpharmacologic approaches may be the more appropriate initial treatment for acute and chronic pain management.
Currently, there is no clear roadmap for a comprehensive approach to pain management that includes evidence-based nonpharmacologic strategies. The goal of this white paper is to outline the role of evidence-based nonpharmacologic strategies for the management of pain and how they can best be integrated with conventional approaches. This integrative pain management approach is in alignment with the stated goals of the reports from the Office of the Army Surgeon General PMTF, NAM, National Academies of Science, and the NIH National Pain Strategy. How pain is assessed, managed and taught to health professionals must be updated. A shift is essential to address the immense deleterious impact that pain and the current system of pain care, including opioid reliance, have on patients, the health system and society.
Read the rest of this Full Text article now!


Leave A Comment