Effect of Intensive Patient Education vs Placebo Patient Education on Outcomes in Patients With Acute Low Back Pain: A Randomized Clinical Trial
Effect of Intensive Patient Education vs Placebo Patient Education on Outcomes in Patients With Acute Low Back Pain: A Randomized Clinical Trial
SOURCE: JAMA Neurol 2019 (Feb 1); 76 (2): 161–169
Adrian C. Traeger, PhD; Hopin Lee, PhD; Markus Hübscher, PhD; Ian W. Skinner, PhD; G. Lorimer Moseley, PhD; Michael K. Nicholas, PhD; Nicholas Henschke, PhD; Kathryn M. Refshauge, PhD; Fiona M. Blyth, PhD; Chris J. Main, PhD; Julia M. Hush, PhD; Serigne Lo, PhD; James H. McAuley, PhD
Neuroscience Research Australia,
Sydney, New South Wales, Australia.
Sydney School of Public Health,
Faculty of Medicine and Health,
The University of Sydney,
Sydney, New South Wales, Australia.
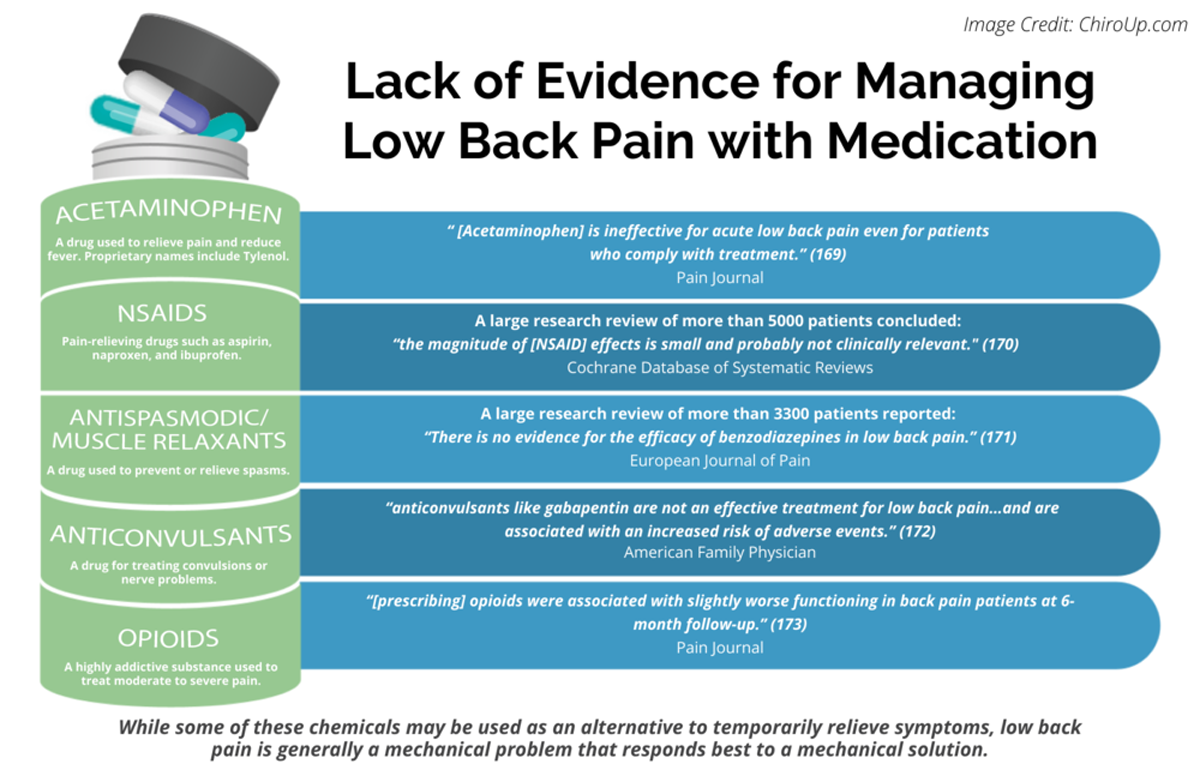
FROM: Pain 2019 (Dec)
FROM: Cochrane Database 2020 (Apr)
FROM: European Journal of Pain 2017 (Feb)
FROM: American Family Physician 2019 (Mar 15)
FROM: Pain 2013 (Jul)
Importance: Many patients with acute low back pain do not recover with basic first-line care (advice, reassurance, and simple analgesia, if necessary). It is unclear whether intensive patient education improves clinical outcomes for those patients already receiving first-line care.
There is more like this @ our:
LOW BACK PAIN Section and the: