Prevalence and Characteristics of Chronic Spinal Pain Patients with Different Hopes (Treatment Goals) for Ongoing Chiropractic Care
Prevalence and Characteristics of Chronic Spinal Pain Patients with Different Hopes (Treatment Goals) for Ongoing Chiropractic Care
SOURCE: J Alternative and Complementary Medicine 2019 (Oct 1); 25 (10): 1015–1025
Patricia M. Herman, ND, PhD, Sarah E. Edgington, MA, Gery W. Ryan, PhD, and Ian D. Coulter, PhD
RAND Corporation,
Santa Monica, CA.
Objectives: The treatment goals of patients successfully using ongoing provider-based care for chronic spinal pain
Design: Multinomial logistical hierarchical linear models were used to examine the characteristics of patients with
Settings/Location: Observational data from a large national sample of patients from 125 chiropractic clinics clustered in 6 U.S. regions.
Subjects: Patients with nonwork-injury-related nonspecific chronic low-back pain (CLBP) and chronic neck pain (CNP).
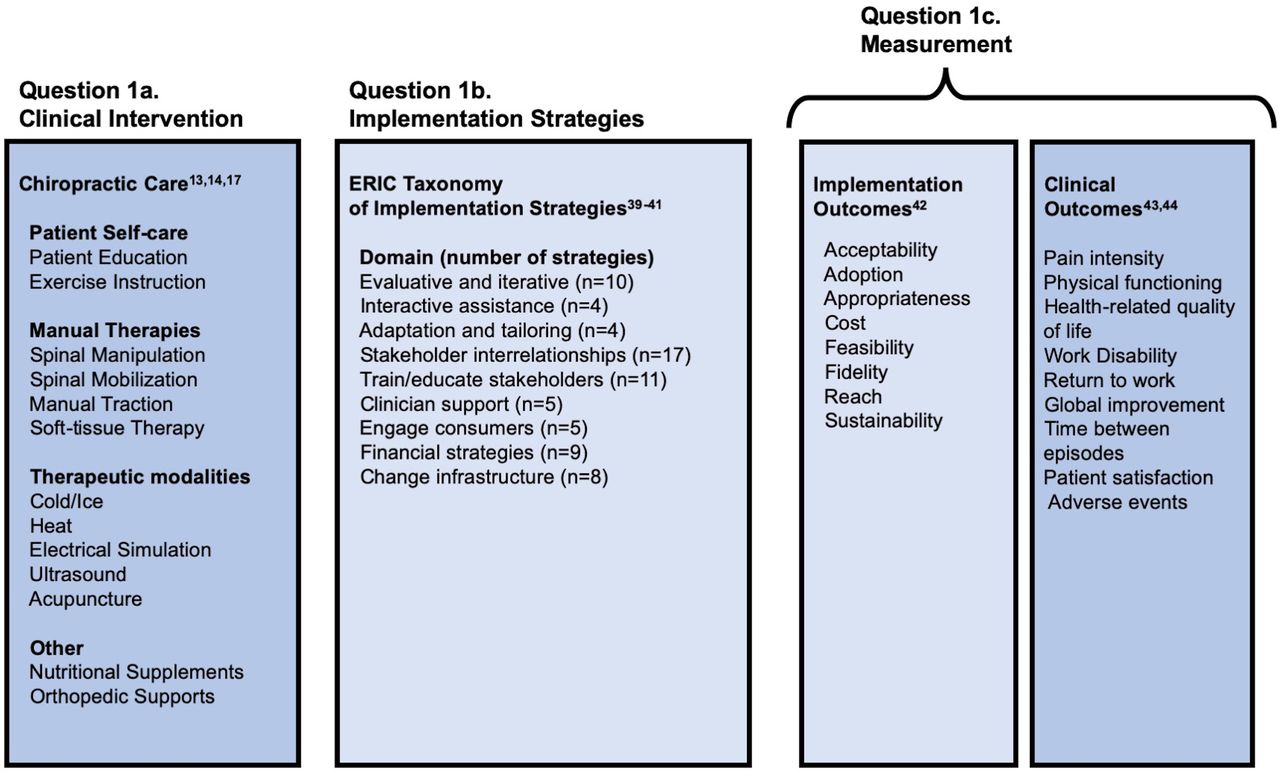
Interventions: All were receiving ongoing chiropractic care.
Outcome measures: Primary outcomes were patient endorsement of one of four goals for their treatment. Explanatory variables included pain characteristics, pain beliefs, goals for mobility/flexibility, demographics, and other psychological variables.
Results: Across our sample of 1614 patients (885 with CLBP and 729 with CNP) just under one-third endorsed a treatment goal of having their pain go away permanently (cure). The rest had goals of preventing their pain from coming back (22% CLBP, 16% CNP); preventing their pain from getting worse (14% CLBP, 12% CNP); or temporarily relieving their pain (31% CLBP, 41% CNP). In univariate analysis across these goals, patients differed significantly on almost all variables. In the multinomial logistic models, a goal of cure was associated with shorter pain duration and more belief in a medical cure; a goal of preventing pain from coming back was associated with lower pain levels; and those with goals of preventing their pain from getting worse or temporarily relieving pain were similar, including in having their pain longer.
There is more like this @ our:
CHRONIC NECK PAIN Page and our
SPINAL PAIN MANAGEMENT Page and our
NON-PHARMACOLOGIC THERAPY Page