Effects of Chiropractic Care on Strength, Balance, and Endurance in Active-Duty U.S. Military Personnel with Low Back Pain
Effects of Chiropractic Care on Strength, Balance, and Endurance in Active-Duty U.S. Military Personnel with Low Back Pain: A Randomized Controlled Trial
SOURCE: J Altern Complement Med 2020 (Jul)
Robert Vining, Cynthia R. Long, Amy Minkalis, M. Ram Gudavalli, Ting Xia, Joan Walter, Ian Coulter, and Christine M. Goertz
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, IA, USA.
Objectives: To investigate whether chiropractic care influences strength, balance, and/or endurance in active-duty United States military personnel with low back pain (LBP).
Design: This study employed a prospective randomized controlled trial using a pragmatic treatment approach. Participants were randomly allocated to 4 weeks of chiropractic care or to a wait-list control. Interventions: Chiropractic care consisted of spinal manipulation, education, advice, and reassurance.
Settings/Location: Naval Air Technical Training Center branch clinic at the Naval Hospital Pensacola Florida.
Subjects: One hundred ten active-duty military personnel 18-40 years of age with self-reported LBP.
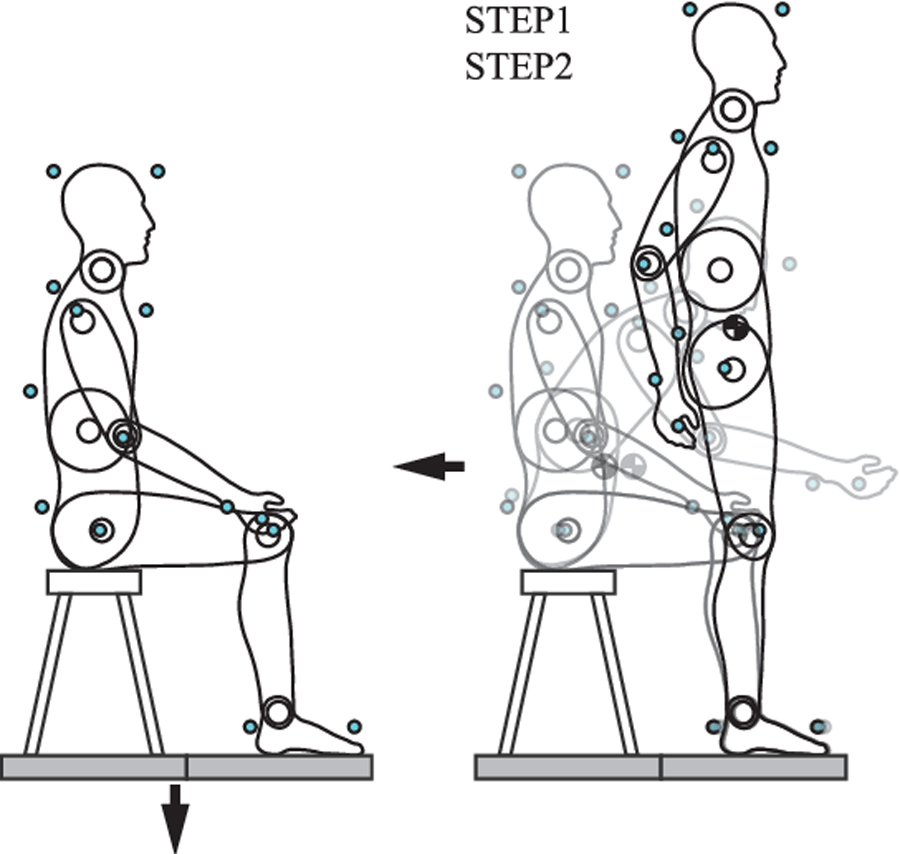
Outcome measures: Isometric pulling strength from a semisquat position was the primary outcome. Secondary outcomes were single-leg balance with eyes open and eyes closed, and trunk muscle endurance using the Biering-Sorensen test. Patient-reported outcomes such as pain severity and disability were also measured. Outcomes were measured at baseline and 4 weeks. Linear mixed-effects regression models over baseline and 4 weeks were used for analysis.
Results: Participants had mean age of 30 years (18-40), 17% were female, 33% were non-white, and 86% reported chronic LBP.
There are more articles like this @ our:
LOW BACK PAIN page and the: