Primary Care for Low Back Pain: We Don’t Know the Half of It
SOURCE: Pain. 2020 (Apr); 161 (4): 663–665
Peter Croft; Saurabb Sharma; Nadine E. Foster
Primary Care Centre Versus Arthritis,
School of Primary, Community and Social Care,
Keele University, Keele, United Kingdom.
Evidence-based medicine helps health care professionals and patients decide best care, drawing on research about effectiveness and safety of interventions. Systematic reviews summarise the evidence; guidelines report consensus between experts (including patients) on interpreting it for everyday practice. Although guideline recommendations are only one component of shared decisions that will vary patient-to-patient, the hoped-for outcome is health benefit for each individual. Guidelines also inform starker decisions by policymakers and health care leaders — for example, when to withdraw approval or funding for a poorly evidenced or harmful intervention. To assess whether all this research-driven activity is useful, 2 questions need answering: how well are guidelines followed in real-life practice and do patients benefit in the long-term?
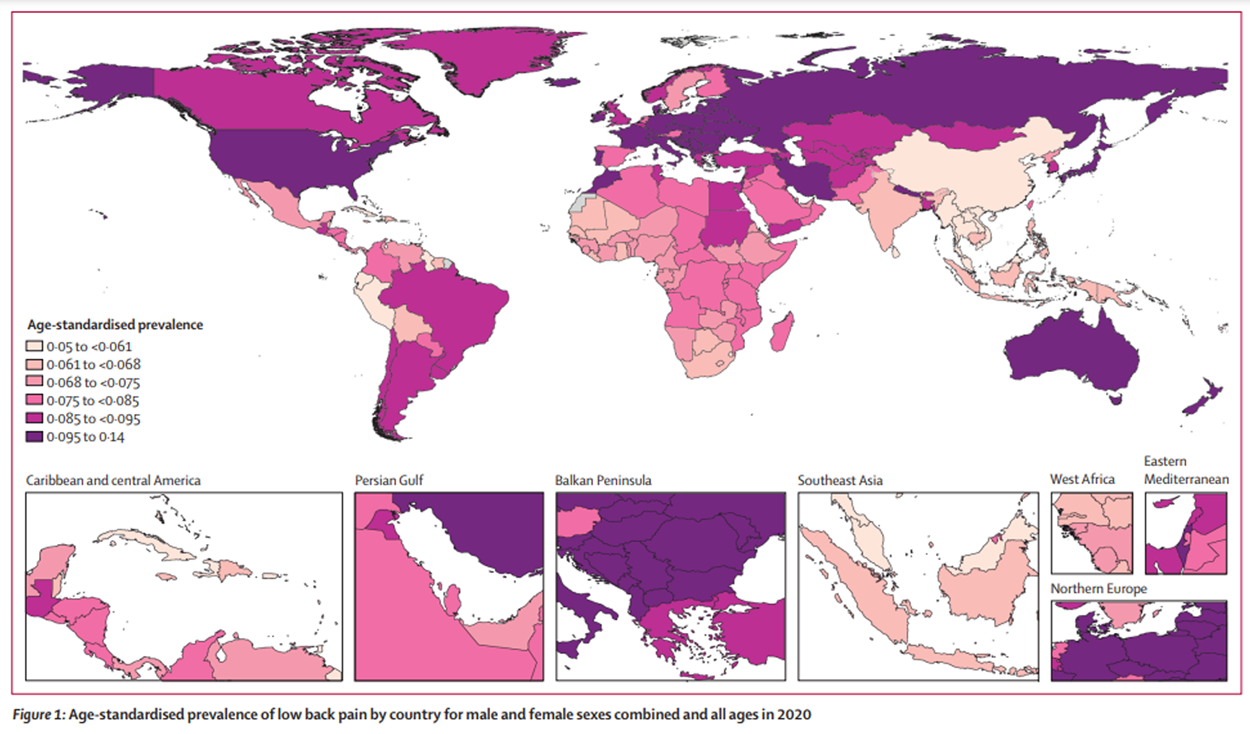
In a new systematic review, Kamper et al. [9] tackle the first question in relation to first-contact care for patients with low back pain provided by family practice and emergency department physicians. (aka “usual medical care”) As the authors state, low back pain has major significance for the international pain community. It is the leading single cause of years lost to disability globally, [17] and there is good evidence for what constitutes best first-contact treatment. [6] The review selected best-quality studies of routine health care data to investigate whether first-contact physicians are putting back pain guidelines into practice (“usual care”).
There are more articles like this @ our:
MEDICARE Page and the:
The results paint a bleak picture: only a minority of patients apparently receive simple positive messages to stay active and exercise, while inappropriate use of analgesia and imaging persists. The review adds to evidence that the care doctors give patients with low back pain is dominated by guideline-discordant interventions that are unnecessary, expensive, and “low-value” (ie, harm is more likely than benefit). [2, 3, 16]
These findings are not entirely unexpected nor, as the authors point out, should blame be placed entirely at the door of front-line physicians. Qualitative studies reveal family practitioners agreeing with guideline conclusions [4] but frustrated in implementing them by factors such as patients with complex needs or lack of resources for behavioural interventions and rehabilitation. [1]
Furthermore, physicians will point to the nuances of individual patients who do not neatly fit the template for guideline recommendations. The review’s authors acknowledge this when discussing the difficulty of measuring “appropriateness” of physician requests for imaging. [9]
The review did not study nonphysician primary care providers. Many such practitioners deliver care aligned with guidelines, such as advice about activity and exercise. More allocation of first-contact low back pain care to professionals such as physical therapists [AND chiropractors] could help to address the problem of inappropriate care. [6] However, although some back care, such as imaging requests by physical therapists, [7] may be more guideline-concordant, a recent systematic review indicated physical therapists have low adherence generally to guidelines for musculoskeletal pain, [18] and a comparison of nurse practitioners and physicians in primary care revealed similar rates of unnecessary imaging requests. [12]
It is increasingly clear that simply expecting individual clinicians to adhere more closely to guidelines is not going to close the evidence-practice gap. Recent articles [2, 3, 16] have argued that effective “high-value” care for patients with low back pain (“benefit more likely than harm”) will only be achieved through large-scale top-down changes across health and social systems (“system strengthening” [2]).
Such changes include engaging policymakers, politicians, and profession leaders to change laws and reimbursement practices; addressing counterproductive commercial pressures; creating incentives for optimal care; providing adequate resources for delivery of guideline care (including digital innovation); shifting professional education and training toward high-value care, including nonpharmacological approaches; dissolving boundaries between health care professions to create unified programmes of care; and changing culture and pain literacy among patients and populations to encourage prevention and positive health activity. [2, 3, 16] The success of such innovations, however, cannot be taken for granted and will need evidence that they bring long-term patient benefit.
Read the rest of this Full Text article now!




Leave A Comment