Association Between Chiropractic Spinal Manipulative Therapy and Benzodiazepine Prescription in Patients with Radicular Low Back Pain: A Retrospective Cohort Study Using Real-world Data From the USA
Association Between Chiropractic Spinal Manipulative Therapy and Benzodiazepine Prescription in Patients with Radicular Low Back Pain: A Retrospective Cohort Study Using Real-world Data From the USA
SOURCE: BMJ Open 2022 (Jun 13); 12 (6): e058769
| OPEN ACCESS |
Robert James Trager, Zachary A Cupler, Kayla J DeLano, Jaime A Perez, Jeffery A Dusek
Connor Whole Health, University Hospitals Cleveland Medical Center,
Cleveland, Ohio, USA
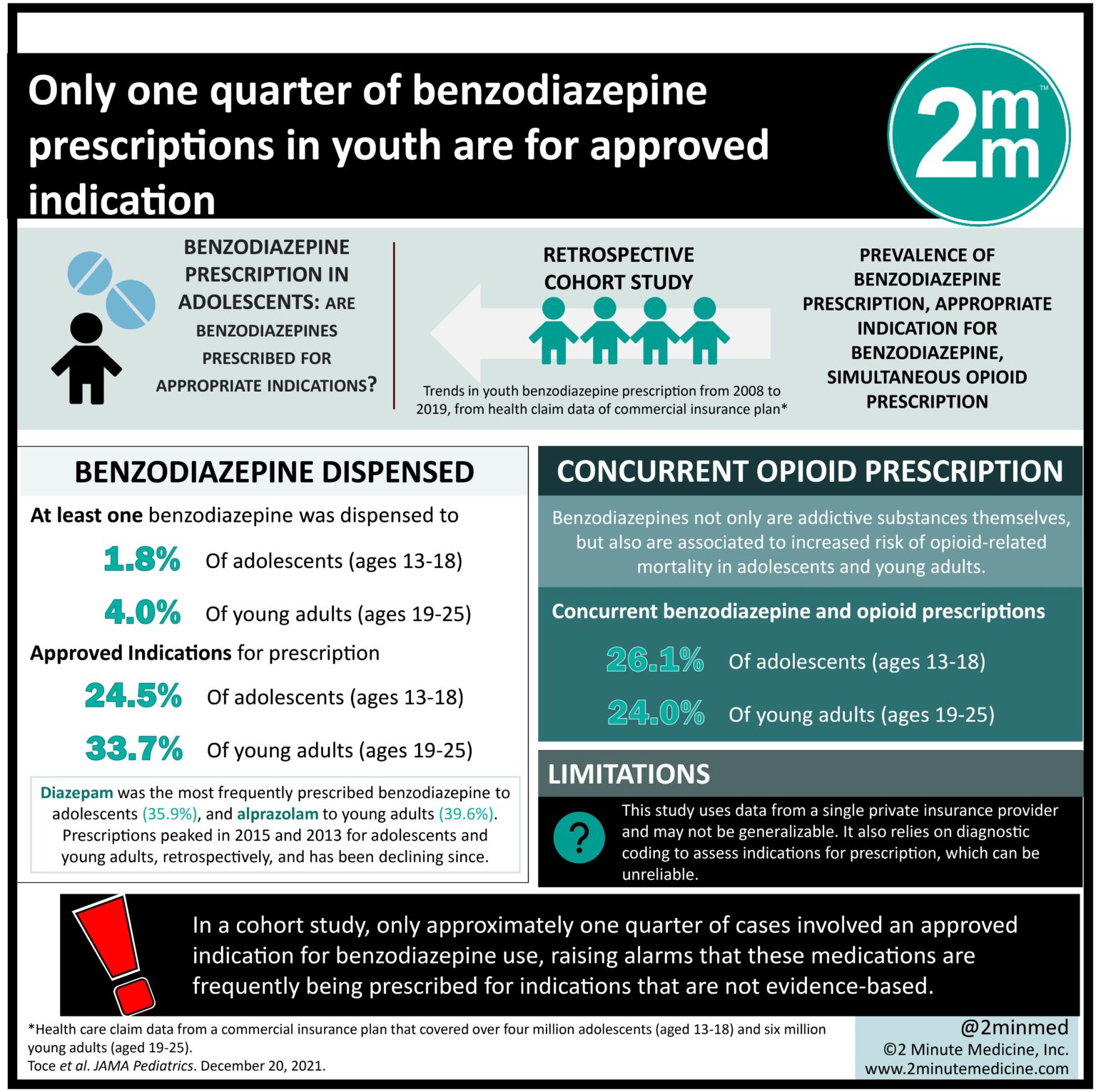
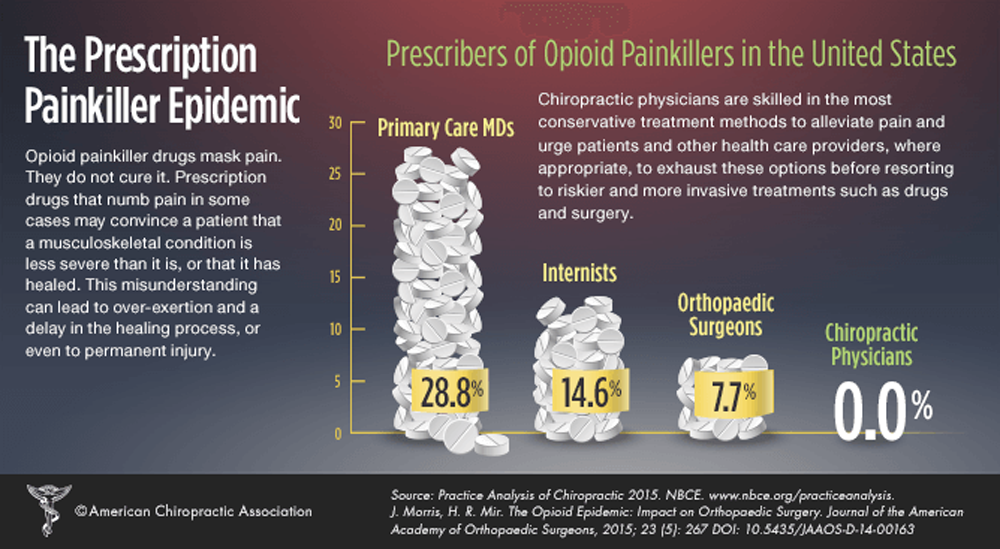
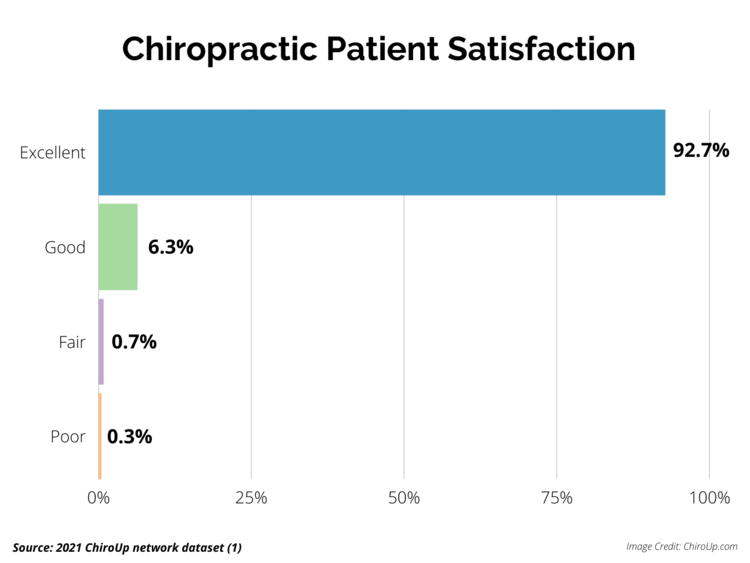
Objectives: Although chiropractic spinal manipulative therapy (CSMT) and prescription benzodiazepines are common treatments for radicular low back pain (rLBP), no research has examined the relationship between these interventions. We hypothesise that utilisation of CSMT for newly diagnosed rLBP is associated with reduced odds of benzodiazepine prescription through 12 months’ follow-up.
Design: Retrospective cohort study.
Setting: National, multicentre 73-million-patient electronic health records-based network (TriNetX) in the USA, queried on 30 July 2021, yielding data from 2003 to the date of query.
Participants: Adults aged 18-49 with an index diagnosis of rLBP were included. Serious aetiologies of low back pain, structural deformities, alternative neurological lesions and absolute benzodiazepine contraindications were excluded. Patients were assigned to cohorts according to CSMT receipt or absence. Propensity score matching was used to control for covariates that could influence the likelihood of benzodiazepine utilisation.
Outcome measures: The number, percentage and OR of patients receiving a benzodiazepine prescription over 3, 6 and 12 months’ follow-up prematching and postmatching.
Results: After matching, there were 9206 patients (mean (SD) age, 37.6 (8.3) years, 54% male) per cohort. Odds of receiving a benzodiazepine prescription were significantly lower in the CSMT cohort over all follow-up windows prematching and postmatching (p<0.0001). After matching, the OR (95% CI) of benzodiazepine prescription at 3 months was 0.56 (0.50 to 0.64), at 6 months 0.61 (0.55 to 0.68) and 12 months 0.67 (0.62 to 0.74). Sensitivity analysis suggested a patient preference to avoid prescription medications did not explain the study findings.
There are more articles like this @ our: