Clinical Classification in Low Back Pain
Clinical Classification in Low Back Pain: Best-evidence Diagnostic Rules Based on Systematic Reviews
SOURCE: BMC Musculoskelet Disord. 2017 (May 12); 18 (1): 188
Tom Petersen, Mark Laslett and
Carsten Juhl
Back Center Copenhagen,
Mimersgade 41, 2200,
Copenhagen N, Denmark.
A clinical decision rule “is a clinical tool that quantifies the individual contributions that various components of the history, physical examination, and basic laboratory results make toward the diagnosis, prognosis, or likely response to treatment in a patient. Clinical decision rules attempt to formally test, simplify, and increase the accuracy of clinicians’ diagnostic and prognostic assessments” [23].This is probably the best and most comprehensive review you will read this year, as it drills down into the findings and treatment of:
Take the time and enjoy this extensive review |
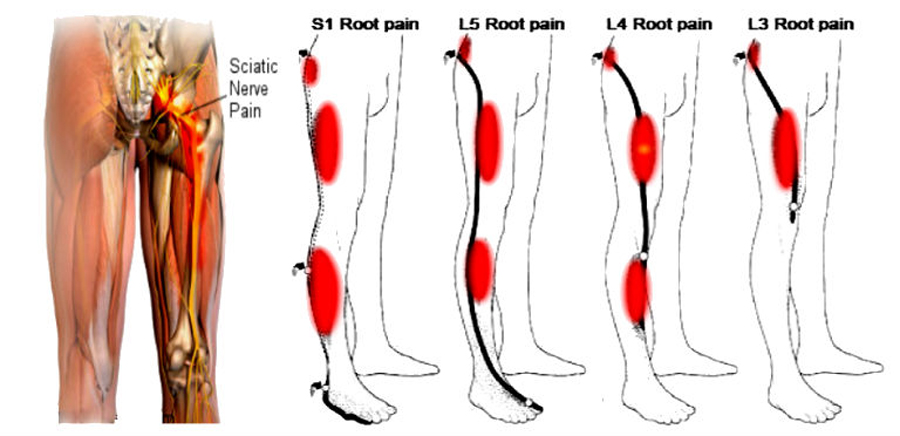
BACKGROUND: Clinical examination findings are used in primary care to give an initial diagnosis to patients with low back pain and related leg symptoms. The purpose of this study was to develop best evidence Clinical Diagnostic Rules (CDR] for the identification of the most common patho-anatomical disorders in the lumbar spine; i.e. intervertebral discs, sacroiliac joints, facet joints, bone, muscles, nerve roots, muscles, peripheral nerve tissue, and central nervous system sensitization.
METHODS: A sensitive electronic search strategy using MEDLINE, EMBASE and CINAHL databases was combined with hand searching and citation tracking to identify eligible studies. Criteria for inclusion were: persons with low back pain with or without related leg symptoms, history or physical examination findings suitable for use in primary care, comparison with acceptable reference standards, and statistical reporting permitting calculation of diagnostic value. Quality assessments were made independently by two reviewers using the Quality Assessment of Diagnostic Accuracy Studies tool. Clinical examination findings that were investigated by at least two studies were included and results that met our predefined threshold of positive likelihood ratio ≥ 2 or negative likelihood ratio ≤ 0.5 were considered for the CDR.
RESULTS: Sixty-four studies satisfied our eligible criteria. We were able to construct promising CDRs for symptomatic intervertebral disc, sacroiliac joint, spondylolisthesis, disc herniation with nerve root involvement, and spinal stenosis. Single clinical test appear not to be as useful as clusters of tests that are more closely in line with clinical decision making.
There are more articles like this @ our:
Clinical Prediction Rule Page and the: