Leg Pain Location and Neurological Signs Relate to Outcomes in Primary Care Patients with Low Back Pain
SOURCE: BMC Musculoskelet Disord. 2017 (Mar 31); 18 (1): 133
Lisbeth Hartvigsen, Lise Hestbaek, Charlotte Lebouef-Yde,
Werner Vach and Alice Kongsted
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmark
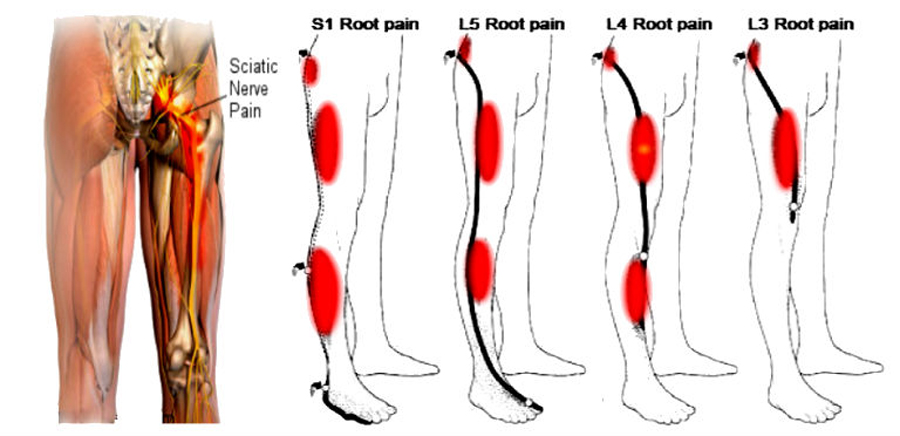
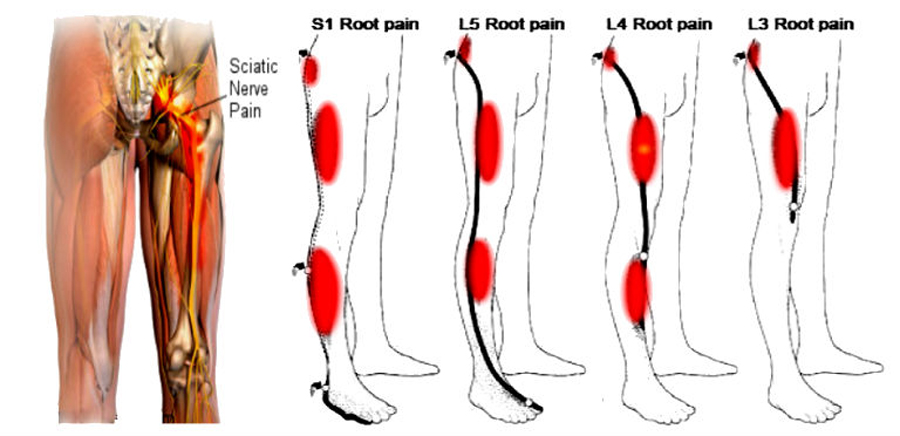
BACKGROUND: Low back pain (LBP) patients with related leg pain and signs of nerve root involvement are considered to have a worse prognosis than patients with LBP alone. However, it is unclear whether leg pain location above or below the knee and the presence of neurological signs are important in primary care patients. The objectives of this study were to explore whether the four Quebec Task Force categories (QTFC) based on the location of pain and on neurological signs have different characteristics at the time of care seeking, whether these QTFC are associated with outcome, and if so whether there is an obvious ranking of the four QTFC on the severity of outcomes.
METHOD: Adult patients seeking care for LBP in chiropractic or general practice were classified into the four QTFC based on self-reported information and clinical findings. Analyses were performed to test the associations between the QTFC and baseline characteristics as well as the outcomes global perceived effect and activity limitation after 2 weeks, 3 months, and 1 year and also 1-year trajectories of LBP intensity.
RESULTS: The study comprised 1,271 patients; 947 from chiropractic practice and 324 from general practice. The QTFC at presentation were statistically significantly associated with most of the baseline characteristics, with activity limitation at all follow-up time points, with global perceived effect at 2 weeks but not 3 months and 1 year, and with trajectories of LBP. Severity of outcomes in the QTFC increased from LBP alone, across LBP with leg pain above the knee and below the knee to LBP with nerve root involvement. However, the variation within the categories was considerable.
There are more articles like this @ our:
Clinical Prediction Rule Page and the:
CONCLUSION: The Quebec Task Force categories (QTFC) identify different LBP subgroups at baseline and there is a consistent ranking of the four categories with respect to outcomes. The differences between outcomes appear to be large enough for the QTFC to be useful for clinicians in the communication with patients. However, due to variation of outcomes within each category individuals’ outcome cannot be precisely predicted from the QTFC alone. It warrants further investigation to find out if the QTFC can improve existing prediction tools and guide treatment decisions.
KEYWORDS: Classification; Cohort studies; Low back pain; Primary care; Quebec Task Force classification; Radiculopathy; Referred leg pain; Sciatica
From the FULL TEXT Article:
Background
Low back pain (LBP) is the leading cause of disability worldwide contributing more than 10 of total years lived with disability [1] and the cost for society is huge. In the United States alone the estimated direct medical cost for all back-related conditions was $253 billion in 2009 to 2011 and back pain resulted in more than 290 million lost workdays [2]. Most of the money is spent on the small minority of patients with persistent work disability [3], and the need for prognostic assessment is highlighted in evidence-based guidelines for nonspecific low back pain in primary care [4]. Feasible assessment tools to identify prognostic indicators are needed that can facilitate clinical decision-making with the ultimate goal of preventing persistent problems and reducing costs.
Many attempts have been made to develop such back pain classification systems and screening tools [5–7]. One tool is the Quebec Task Force (QTF) classification of spinal disorders, proposed in 1987 [7]. The classification in its original form includes 11 categories.
Categories 1 to 3 are based on the location of pain:
Read the rest of this Full Text article now!

Leave A Comment