Impact of Chiropractic Care on Use of Prescription Opioids
Impact of Chiropractic Care on Use of Prescription Opioids in Patients with Spinal Pain
SOURCE: Pain Med. 2020 (Mar 6) [Epub]
James M. Whedon, DC, MS, Andrew W. J. Toler, MS, Louis A. Kazal, MD, Serena Bezdjian, PhD, Justin M. Goehl, DC, MS et al.
Southern California University of Health Sciences,
Whittier, California.
OBJECTIVE: Utilization of nonpharmacological pain management may prevent unnecessary use of opioids. Our objective was to evaluate the impact of chiropractic utilization upon use of prescription opioids among patients with spinal pain.
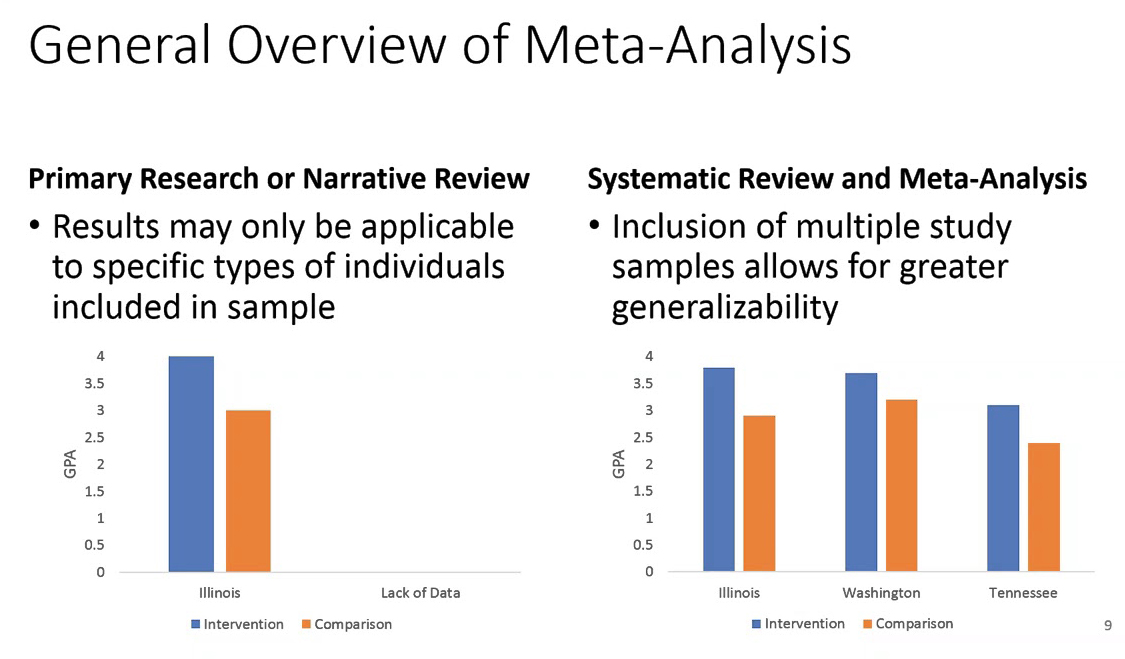
DESIGN AND SETTING: We employed a retrospective cohort design for analysis of health claims data from three contiguous states for the years 2012-2017.
SUBJECTS: We included adults aged 18-84 years enrolled in a health plan and with office visits to a primary care physician or chiropractor for spinal pain. We identified two cohorts of subjects: Recipients received both primary care and chiropractic care, and nonrecipients received primary care but not chiropractic care.
METHODS: We performed adjusted time-to-event analyses to compare recipients and nonrecipients with regard to the risk of filling an opioid prescription. We stratified the recipient populations as: acute (first chiropractic encounter within 30 days of diagnosis) and nonacute (all other patients).
There are more articles like this @ our: