Benefits and Harms of Spinal Manipulative Therapy for the Treatment of Chronic Low Back Pain: Systematic Review and Meta-analysis of Randomised Controlled Trials
SOURCE: British Medical Journal 2019 (Mar 13)
Sidney M Rubinstein, Annemarie de Zoete, Marienke van Middelkoop, Willem J J Assendelft, Michiel R de Boer, and Maurits W van Tulder
Department of Health Sciences,
Faculty of Science,
Vrije Universiteit Amsterdam,
De Boelelaan 1085, 1081HV
Amsterdam, Netherlands
OBJECTIVE: To assess the benefits and harms of spinal manipulative therapy (SMT) for the treatment of chronic low back pain.
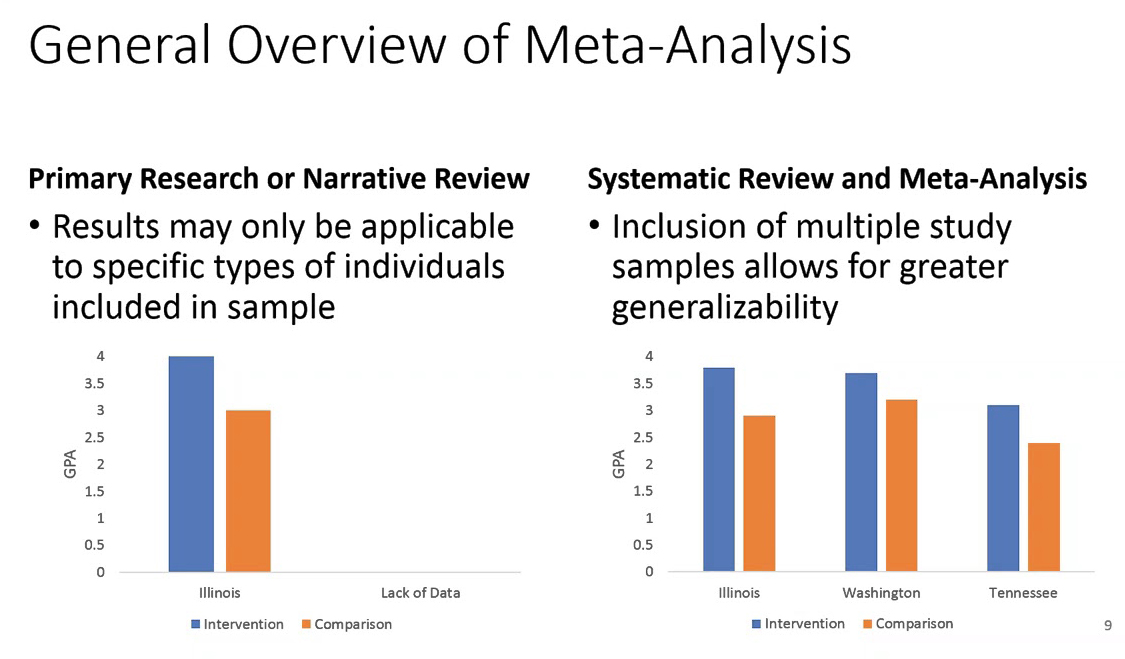
DESIGN: Systematic review and meta-analysis of randomised controlled trials.
DATA SOURCES: Medline, PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), CINAHL, Physiotherapy Evidence Database (PEDro), Index to Chiropractic Literature, and trial registries up to 4 May 2018, including reference lists of eligible trials and related reviews.
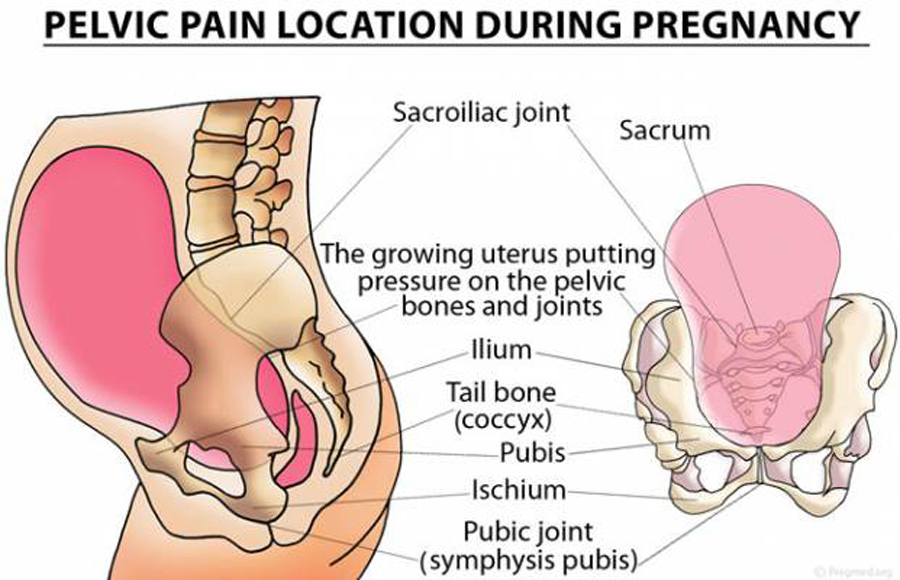
ELIGIBILITY CRITERIA FOR SELECTING STUDIES: Randomised controlled trials examining the effect of spinal manipulation or mobilisation in adults (≥18 years) with chronic low back pain with or without referred pain. Studies that exclusively examined sciatica were excluded, as was grey literature. No restrictions were applied to language or setting.
REVIEW METHODS: Two reviewers independently selected studies, extracted data, and assessed risk of bias and quality of the evidence.
There are more articles like this @ our:
The effect of SMT was compared with recommended therapies, non-recommended therapies, sham (placebo) SMT, and SMT as an adjuvant therapy. Main outcomes were pain and back specific functional status, examined as mean differences and standardised mean differences (SMD), respectively. Outcomes were examined at 1, 6, and 12 months. Quality of evidence was assessed using GRADE. A random effects model was used and statistical heterogeneity explored.
RESULTS: 47 randomised controlled trials including a total of 9211 participants were identified, who were on average middle aged (35-60 years). Most trials compared SMT with recommended therapies. Moderate quality evidence suggested that SMT has similar effects to other recommended therapies for short term pain relief (mean difference -3.17, 95% confidence interval -7.85 to 1.51) and a small, clinically better improvement in function (SMD -0.25, 95% confidence interval -0.41 to -0.09). High quality evidence suggested that compared with non-recommended therapies SMT results in small, not clinically better effects for short term pain relief (mean difference -7.48, -11.50 to -3.47) and small to moderate clinically better improvement in function (SMD -0.41, -0.67 to -0.15). In general, these results were similar for the intermediate and long term outcomes as were the effects of SMT as an adjuvant therapy. Evidence for sham SMT was low to very low quality; therefore these effects should be considered uncertain. Statistical heterogeneity could not be explained. About half of the studies examined adverse and serious adverse events, but in most of these it was unclear how and whether these events were registered systematically. Most of the observed adverse events were musculoskeletal related, transient in nature, and of mild to moderate severity. One study with a low risk of selection bias and powered to examine risk (n=183) found no increased risk of an adverse event (relative risk 1.24, 95% confidence interval 0.85 to 1.81) or duration of the event (1.13, 0.59 to 2.18) compared with sham SMT. In one study, the Data Safety Monitoring Board judged one serious adverse event to be possibly related to SMT.
CONCLUSION: SMT produces similar effects to recommended therapies for chronic low back pain, whereas SMT seems to be better than non-recommended interventions for improvement in function in the short term. Clinicians should inform their patients of the potential risks of adverse events associated with SMT.
From the FULL TEXT Article
Introduction
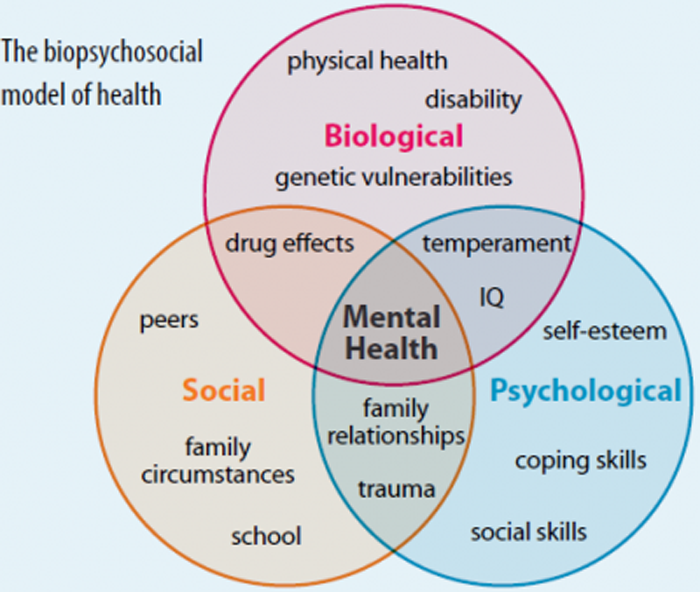
Low back pain is a common and disabling disorder. [1] Adequate treatment of low back pain is therefore important for patients, clinicians, and healthcare policy makers. Spinal manipulative therapy (SMT) is widely used to treat low back pain and has been examined in numerous randomised controlled trials of varying methodological quality and size, with varying results. These trials have been summarised in systematic reviews, including an earlier review of ours, and the results form the basis for recommendations in clinical guidelines. [2–5]
The effectiveness of SMT for the treatment of chronic low back pain and therefore recommendations in international guidelines for the use of non-drug interventions in the treatment of non-specific low back pain, are not without dispute.6 In some countries, SMT is considered a first line treatment option, [3] whereas in others it is recommended as a component of a broader treatment package including exercise, [5] or is not included or mentioned at all. [4] The most recent summary of these guidelines suggests that SMT should be considered a second line or adjuvant treatment option, after exercise or cognitive behavioural therapy. [7]
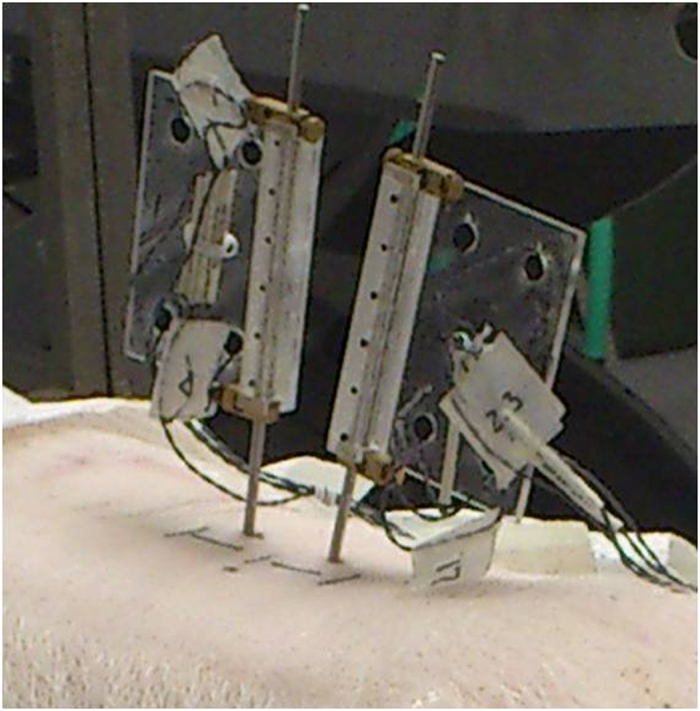
In this review, we consider SMT to represent any hands-on treatment of the spine, including both mobilisation and manipulation. Mobilisations use low grade velocity, small or large amplitude passive movement techniques within the patient’s range of motion and control, whereas manipulation uses a high velocity impulse or thrust applied to a synovial joint over a short amplitude at or near the end of the passive or physiological range of motion. [8] This is often accompanied by an audible crack, resulting from cavitation of the joint.
Read the rest of this Full Text article now!


Leave A Comment