Chiropractic Integration Within a Community Health Centre: A Cost Description and Partial Analysis of Cost-utility from the Perspective of the Institution
SOURCE: J Can Chiropr Assoc. 2019 (Aug); 63 (2): 64–79
Peter C Emary, DC, MSc, Amy L Brown, DC, Douglas F Cameron, DC, and Alexander F Pessoa, DC
Private Practice,
Cambridge, ON, Canada.
OBJECTIVE: To evaluate costs and consequences of a new back pain service provided by chiropractors integrated into a Community Health Centre in Cambridge, Ontario. The study sample included 95 consecutive patients presenting between January 2014 to January 2016 with a mixture of sub-acute and chronic back pain.
METHODS: A secondary cost-utility analysis was performed and conducted from the perspective of the healthcare institution. Cost-utility was calculated as cost per quality-adjusted life year (QALY) gained over a time horizon of 90 days.
RESULTS: According to the EuroQol 5 Domain questionnaire, nearly 70% of patients improved. The mean number of treatment sessions was 8.4, and an average of 0.21 QALYs were gained at an average cost per QALY of $1,042. Seventy-seven percent of patients did not visit their primary care provider over the 90-day period, representing potential cost savings to the institution of between $2,022.23 and $6,135.82.
There are more articles like this @ our:
Conclusions: Adding chiropractic care to usual medical care was associated with improved outcomes at a reasonable cost in a sample of complex patients with sub-acute and chronic back pain. Future comparative cost-effectiveness studies are needed.
KEYWORDS: chiropractic; community health centres; cost analysis; health services research
From the FULL TEXT Article:
Introduction
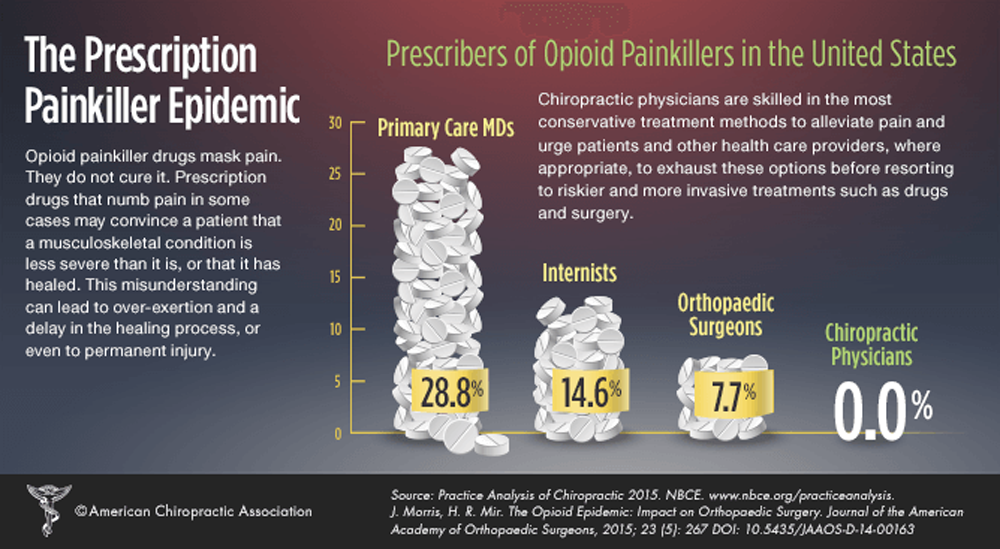
The efficacy for chiropractic care including manipulative therapy in treating patients with spine-related pain has been established. [1–3] Moreover, clinical trials have shown greater efficacy when chiropractic treatment is added to usual medical care in managing patients with these conditions. [4, 5] Chiropractic care also has the potential to be cost-effective, as chiropractors typically use a conservative (i.e. non-pharmacological, non-surgical) approach. In fact, studies have shown that when managed by a chiropractor, even when controlling for confounding factors, patients tend to have fewer advanced medical procedures including opioids and referrals for diagnostic imaging, injections, or spinal surgery. [6–8]
Although chiropractic care has been suggested as a cost-effective alternative to the medical management of spine-related pain disorders9, the evidence for economic evaluations of chiropractic treatment compared with, or added to, medical care is inconclusive. [10] Regardless, back and neck pain remain prevalent and costly in society. The socioeconomic burden of these disorders, in terms of health resource utilization and economic costs (e.g. lost productivity), is particularly high among vulnerable populations. [9, 11] In Canada, such populations commonly receive health care services at the primary care level within Community Health Centres (CHCs). [12]
CHCs are non-profit, publicly funded and community-governed organizations that promote health, illness prevention, and community development. [12] These centres employ multidisciplinary teams of health professionals that traditionally include medical doctors, nurse practitioners, registered nurses, dieticians, social workers, and community health workers. CHCs are distinct from other primary care centres in that they serve the needs of complex patient populations, typically including younger individuals, the socioeconomically disadvantaged, people with severe mental health or addiction issues (e.g. opioid over-use), and those with various other co-morbidities. [12, 13] Musculoskeletal disorders including chronic back pain are also prevalent among these groups. [9, 14, 15] To improve the management of these patients, particularly in the clinical area of low back pain, a growing number of Ontario CHCs have been adding chiropractic care to their existing medical services. Some of these programs have been voluntary [16] and some have been funded as pilot projects by the Ontario Ministry of Health and Long-Term Care
[14, 17]
In line with such integration, the examination of costs and cost-effectiveness of chiropractic care has become one of the top research priorities for the chiropractic profession in Canada. [18] In 2017, a pilot project was conducted to evaluate a new integrated chiropractic back pain program at the Langs CHC in Cambridge, Ontario. [16, 19] The main findings included patient-reported improvements in back pain intensity, disability and health-related quality of life, high levels of satisfaction, and reduced primary care provider visits and analgesic use with this service. [16] Although such findings suggest potential for health cost savings, a formal economic evaluation of this project was not undertaken. Others have found similar outcomes [14, 15, 17] yet few studies have examined the costs associated with chiropractic integration into primary healthcare settings, including within CHCs. Moreover, no studies have explored whether the implementation of these programs is cost-effective from the institutional point of view. As such, the purpose of the current study was to conduct a secondary analysis of the aforementioned program16 using an economic evaluation design completed from the perspective of the Langs CHC. [19] Resource utilization and costs at the CHC from the health system perspective will be measured in a future study.
Read the rest of this Full Text article now!


Leave A Comment