Integration of Doctors of Chiropractic Into Private Sector Health Care Facilities in the United States: A Descriptive Survey
SOURCE: J Manipulative Physiol Ther. 2018 (Feb); 41 (2): 149–155
Stacie A. Salsbury, PhD, RN, Christine M. Goertz, DC, PhD, Elissa J. Twist, DC, MS, Anthony J. Lisi, DC
Palmer Center for Chiropractic Research,
Palmer College of Chiropractic,
Davenport, Iowa.

OBJECTIVE: The purpose of this study was to describe the demographic, facility, and practice characteristics of doctors of chiropractic (DCs) working in private sector health care settings in the United States.
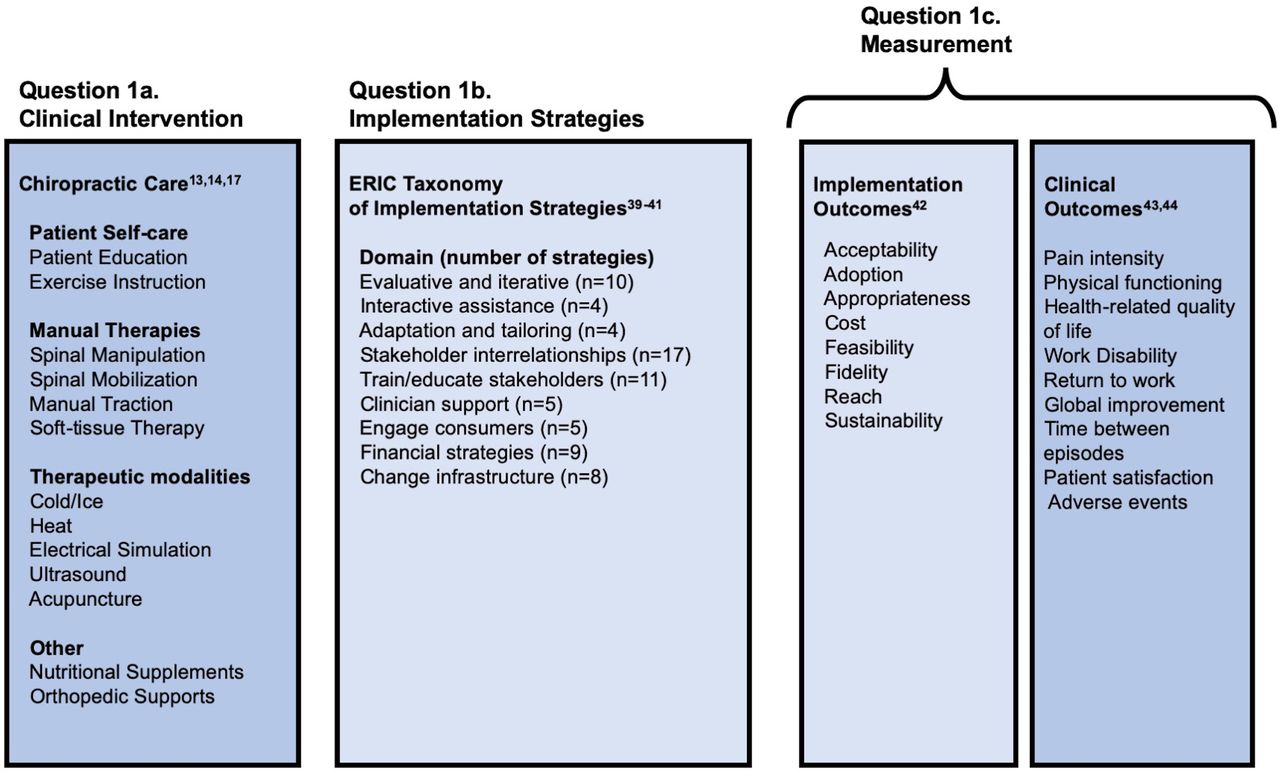
METHODS: We conducted an online, cross-sectional survey using a purposive sample of DCs (n = 50) working in integrated health care facilities. The 36-item survey collected demographic, facility, chiropractic, and interdisciplinary practice characteristics, which were analyzed with descriptive statistics.
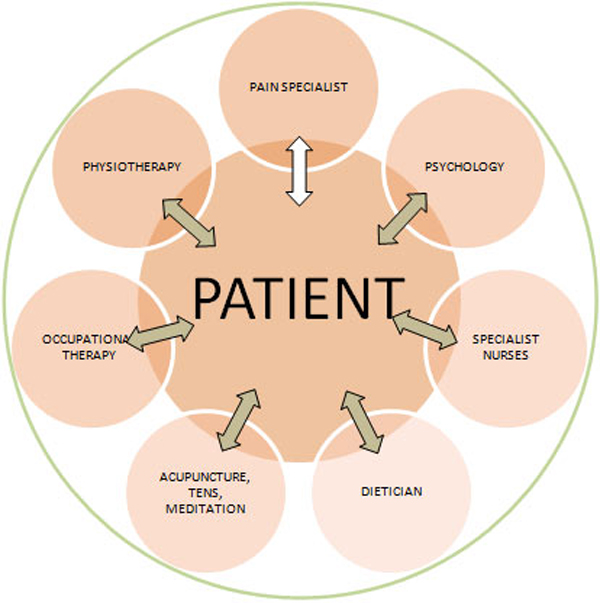
RESULTS: The response rate was 76% (n = 38). Most respondents were men and mid-career professionals with a mean 21 years of experience in chiropractic. Doctors of chiropractic reported working in hospitals (40%), multispecialty offices (21%), ambulatory clinics (16%), or other (21%) health care settings. Most (68%) were employees and received salary compensation (59%). The median number of DCs per setting was 2 (range 1–8). Most DCs used the same health record as medical staff and worked in the same clinical setting. More than 60% reported co-management of patients with medical professionals. Integrated DCs most often received and made referrals to primary care, physical medicine, pain medicine, orthopedics, and physical or occupational therapy. Although in many facilities the DCs were exclusive providers of spinal manipulation (43%), in most, manipulative therapies also were delivered by physical therapists and osteopathic or medical physicians. Informal face-to-face consultations and shared health records were the most common communication methods.
There are more articles like this @ our:
CONCLUSIONS: Doctors of chiropractic are working in diverse medical settings within the private sector, in close proximity and collaboration with many provider types, suggesting a diverse role for chiropractors within conventional health care facilities.
KEYWORDS: Chiropractic; Delivery of Health Care; Integrative Medicine; Interprofessional Relations; Manipulation, Spinal; Private Sector
From the FULL TEXT Article:
Introduction
Chiropractic care has been reported to have effectiveness for managing musculoskeletal disorders, particularly spine-related pain and disability. [1, 2] Over the past 2 decades, large public sector health care delivery systems in the United States, including the Department of Defense and Department of Veterans Affairs (VA), have integrated chiropractic care into their offered services. [3–5] Private sector medical settings, ranging from small primary care clinics to large health care systems in the United States, have introduced chiropractic care. [6–10] A survey by the National Board of Chiropractic Examiners Practice Analysis of Chiropractic reported that 9% of doctors of chiropractic (DCs) practice in settings other than chiropractic offices, including 7.8% who work in an “integrated health care facility,” with 3.6% of those surveyed identifying that they hold hospital staff privileges. [11]
The health care literature rarely describes characteristics of chiropractic practice in the US private sector; most reports are single-site case studies. [7, 8, 12, 13] Consequently, data are lacking on the structures and processes supporting the integration of chiropractic services into these health care facilities. Davis et al offered their experiences establishing chiropractic services in a primary care clinic in rural Vermont, noting the integrated model enhanced patient engagement, care coordination and referral between disciplines, and trust among providers. [7] Their practice model required considerable interprofessional education, was limited by insurance reimbursements, and necessitated negotiation of boundaries between chiropractic and physical therapy services. [7] Branson reflected on a 10-year period of chiropractic integration into a private hospital system in an urban setting in Minnesota. [8]
The growing interest in complementary services within the community, long-term professional relationships, an increasing evidence-base for chiropractic care, availability of adequate physical space, and the creation of an interdisciplinary program for spine care served as key facilitators of chiropractic integration within that health system. [8] Pfefer et al described the integration of chiropractic care into a free safety-net clinic as a specialty service in suburban Kansas, noting the requirements for referral from clinic medical staff, difficulties with adding chiropractic forms to the electronic health record, and problems delivering health promotion counseling as a result of scheduling limitations. [12] Paskowski et al described the implementation of a hospital-based spine care pathway that included DCs on a multidisciplinary team in suburban Massachusetts. [13] Internal development that supported the project included the creation of an evidence-based pathway, buy-in from team members to adopt national back pain guidelines, initiation of clinical outcome measures across settings, and staff educational programs, with external development enhanced by educational outreach to primary care and specialty clinicians. [13]
A survey of American Chiropractic Association members indicated that 17% of 1,142 members reported working in integrated settings ranging from private group practices (59%), ambulatory care/outpatient clinics (15%), hospitals and medical centers (13%), and other types of facilities (11%), with 46% of these facilities located in the private sector. [6] Respondents reported that they served as musculoskeletal specialists and reported higher rates of referral to and from medical doctors (MDs) than those DCs who worked in nonintegrated settings. However, many DCs faced barriers to full participation in the health care team, which included not documenting care in the same clinical record or a lack of referrals from some medical providers. [6]
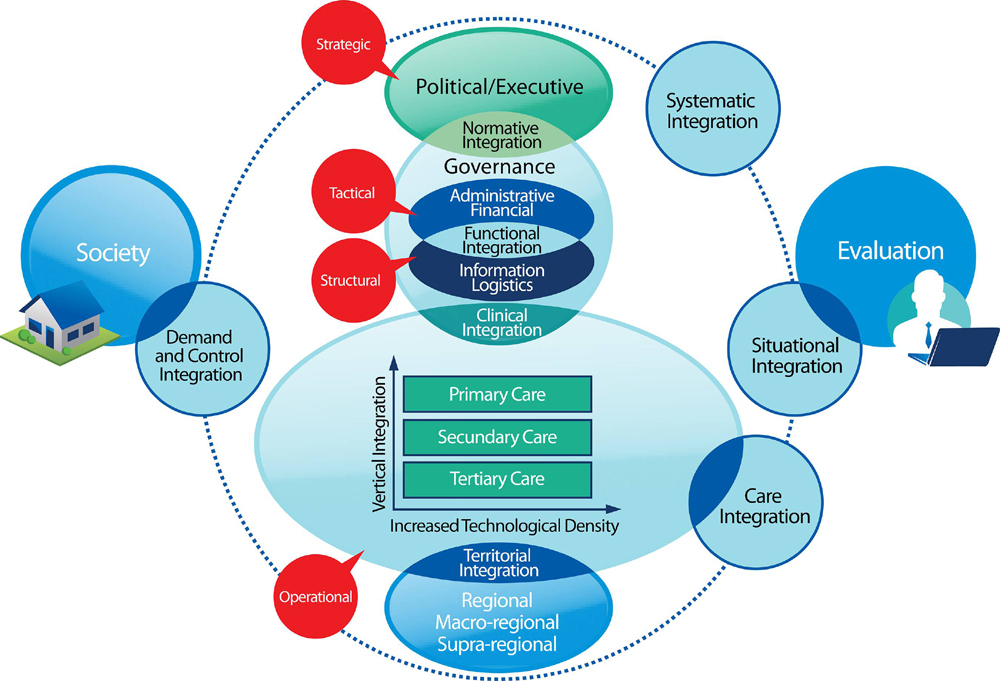
Health care systems are highly complex and differ considerably in their structures, processes, and outcomes. Thus, a better understanding of the existing models and characteristics of chiropractic practice in private medical settings is a key precursor to inclusion of chiropractic services in this sector and improved health care quality for persons with spine-related conditions. [14] Public sector settings, such as within the VA, have facility-level variations in chiropractic integration in terms of planning and implementation processes, clinic features, patient demography, and organizational supports. [15] Similar variations in the structures and processes of chiropractic service integration in community-based health care settings is anticipated, but these are not well documented in the literature. Therefore, the purpose of this study was to describe the demographic, facility, and practice characteristics of select DCs working in private sector health care settings in the United States.
Read the rest of this Full Text article now!

Leave A Comment