Validity and Reliability of Clinical Prediction Rules used to Screen for Cervical Spine Injury in Alert Low-risk Patients with Blunt Trauma to the Neck: Part 2. A Systematic Review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
SOURCE: European Spine Journal 2017 (Sep 22) [Epub]
N. Moser, N. Lemeunier, D. Southerst, H. Shearer, K. Murnaghan, D. Sutton, P. Cote
Division of Graduate Education and Research,
Canadian Memorial Chiropractic College (CMCC),
6100 Leslie Street,
Toronto, ON, Canada.
PURPOSE: To update findings of the 2000-2010 Bone and Joint Decade Task Force on Neck Pain and its Associated Disorders (Neck Pain Task Force) on the validity and reliability of clinical prediction rules used to screen for cervical spine injury in alert low-risk adult patients with blunt trauma to the neck.
METHODS: We searched four databases from 2005 to 2015. Pairs of independent reviewers critically appraised eligible studies using the modified QUADAS-2 and QAREL criteria. We synthesized low risk of bias studies following best evidence synthesis principles.
RESULTS: We screened 679 citations; five had a low risk of bias and were included in our synthesis. The sensitivity of the Canadian C-spine rule ranged from 0.90 to 1.00 with negative predictive values ranging from 99 to 100%. Inter-rater reliability of the Canadian C-spine rule varied from k = 0.60 between nurses and physicians to k = 0.93 among paramedics. The inter-rater reliability of the Nexus Low-Risk Criteria was k = 0.53 between resident physicians and faculty physicians.
There are more articles like this @ our:
CONCLUSIONS: Our review adds new evidence to the Neck Pain Task Force and supports the use of clinical prediction rules in emergency care settings to screen for cervical spine injury in alert low-risk adult patients with blunt trauma to the neck. The Canadian C-spine rule consistently demonstrated excellent sensitivity and negative predictive values. Our review, however, suggests that the reproducibility of the clinical predictions rules varies depending on the examiners level of training and experience.
KEYWORDS: Canadian C-spine rule; Clinical prediction rule; Neck pain; Nexus low-risk criteria; Reliability; Validity
From the FULL TEXT Article:
Introduction
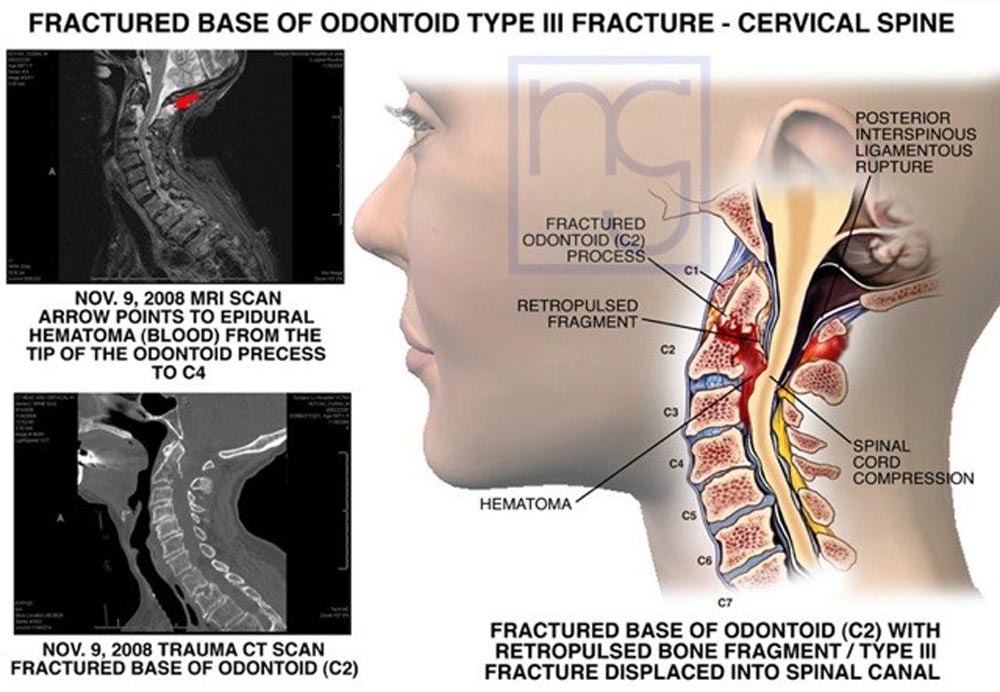
The incidence of a potentially serious cervical spine injury, including cervical spine fracture, dislocation, and ligamentous instability in the Norwegian population, is an estimated 16.5/100,000/year. [1] In the United States, more than a million patients are assessed each year. [2] Failure to diagnose these injuries in a timely manner may have significant consequences, including spinal cord injury and even death. [3] Thus, highly sensitive and reliable assessment methods are required to screen patients who are at risk of serious cervical spine injury.
The primary focus of an assessment for patients with acute neck pain following blunt trauma is to rule out the presence of major pathology, such as fractures and dislocations. [4] Assessment of the anatomical integrity of the cervical spine involves diagnostic imaging, such as plain radiography, computed tomography, or magnetic resonance imaging. However, relying on these procedures is an inefficient practice. [5–8] More than 98% of all cervical spine radiographs ordered following acute blunt trauma are negative for fracture. [6, 9–11] This low diagnostic yield is associated with significant costs and places a significant strain on health care resources]. [5, 12, 13] Furthermore, patients are exposed to potentially harmful radiation when imaging may not be clinically indicated. [14]
Clinical practice guidelines for the assessment of neck pain [15, 16] advocate for the use of clinical prediction rules to identify those at low risk of serious cervical spine injuries. Clinical prediction rules serve as a decision matrix, incorporating three or more variables from the patient’s history, physical examination, and/or simple diagnostic tests. Their intent is to guide the diagnostic and treatment decision-making process. [17, 18]
Read the rest of this Full Text article now!

Leave A Comment