Low Back Pain: A Major Global Problem For Which
Low Back Pain: A Major Global Problem For Which the Chiropractic Profession Needs to Take More Care
SOURCE: Chiropractic & Manual Therapies 2018 (Jun 25); 26: 28
Simon D. French, Aron S. Downie and Bruce F. Walker
Department of Chiropractic,
Faculty of Science and Engineering,
Macquarie University,
Sydney, Australia
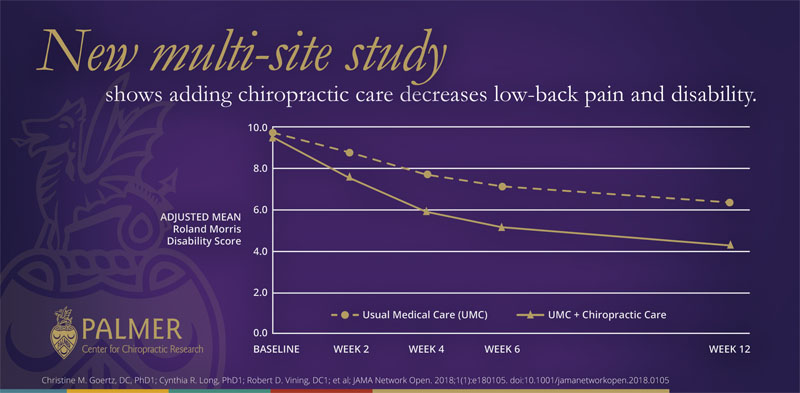
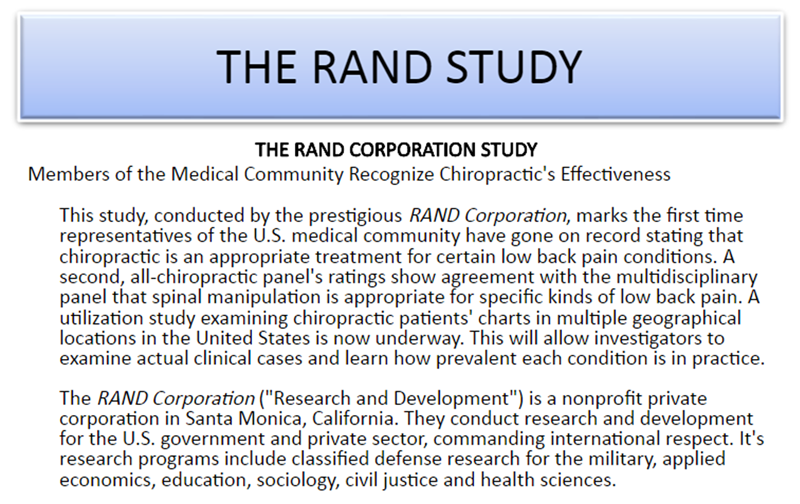
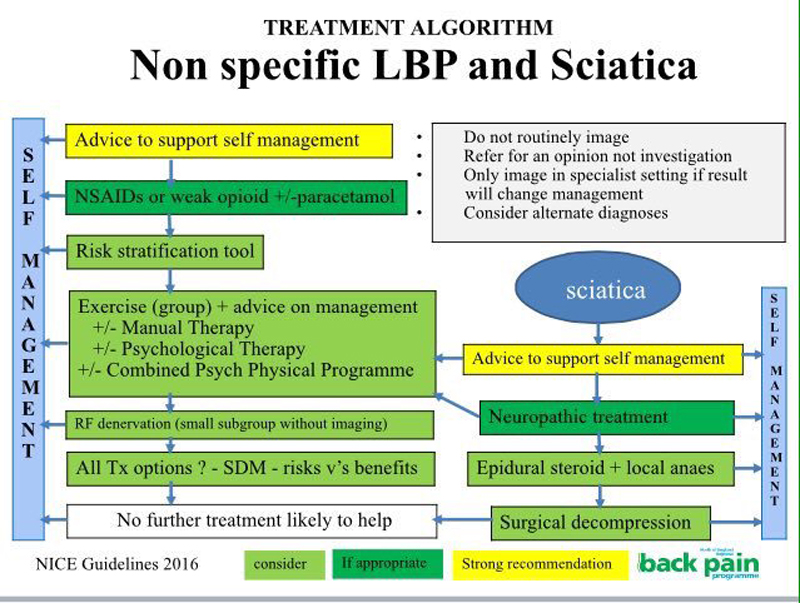
An important series of papers have been published in the Lancet. These papers provide a comprehensive update for the major global problem of low back pain, and the challenges that low back pain presents to healthcare practitioners and policy makers. Chiropractors are well placed to reduce the burden of low back pain, but not all that chiropractors do is supported by robust, contemporary evidence. This commentary summarises the Lancet articles. We also make suggestions for how the chiropractic profession should most effectively help people with low back pain by implementing practices supported by high quality evidence.
This is just one article from a series of 4:
From the Full-Text Article
Background
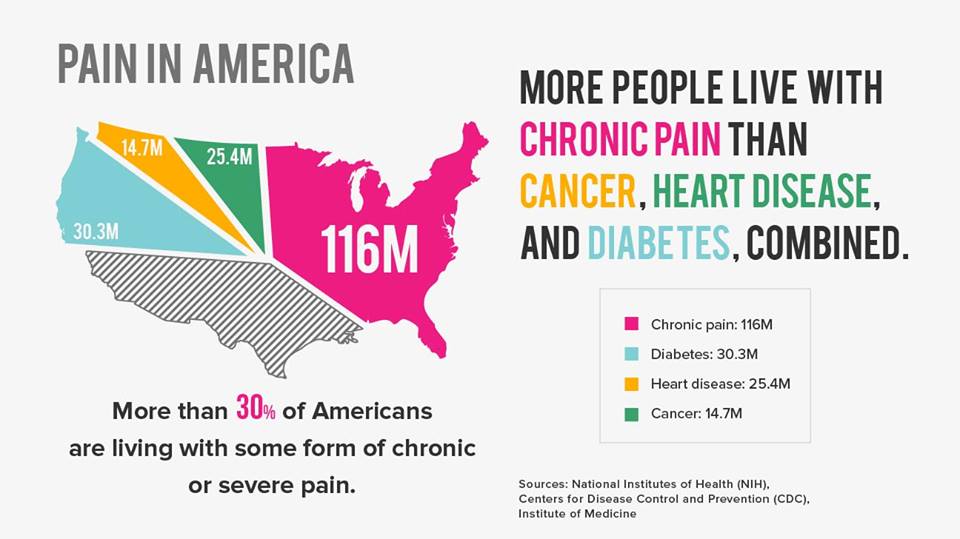
Low back pain is a major global problem and it is getting worse. [1] An important series of articles in the journal Lancet, authored by world leading authorities on low back pain evidence, has drawn international attention to how enormous the problem is. The Lancet authors also discussed how low back pain is being poorly managed by healthcare systems around the globe, including emerging issues in low and middle-income countries. [2–4] This commentary will summarise the main findings of these Lancet papers, and provide some suggestions for how the chiropractic profession should respond to the global challenge that is low back pain.
The Lancet papers
There are more articles like this @ our: