Cost-effectiveness of Spinal Manipulation, Exercise
Cost-effectiveness of Spinal Manipulation, Exercise, and Self-management for Spinal Pain Using an Individual Participant Data Meta-analysis Approach: A Study Protocol
SOURCE: Chiropractic & Manual Therapies 2018 (Nov 13); 26: 46
Brent Leininger, Gert Bronfort, Roni Evans, James Hodges, Karen Kuntz and John A. Nyman
Integrative Health & Wellbeing Research Program,
Earl E. Bakken Center for Spirituality & Healing,
University of Minnesota,
420 Delaware St SE,
Minneapolis, MN 55455, USA
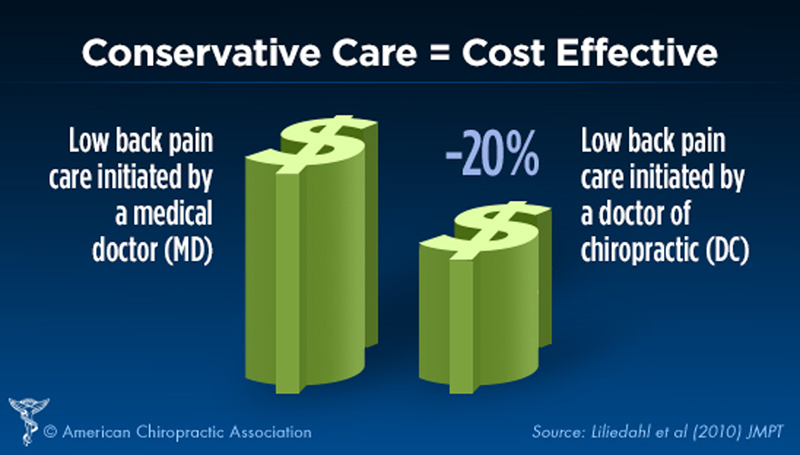
Background Spinal pain is a common and disabling condition with considerable socioeconomic burden. Spine pain management in the United States has gathered increased scrutiny amidst concerns of overutilization of costly and potentially harmful interventions and diagnostic tests. Conservative interventions such as spinal manipulation, exercise and self-management may provide value for the care of spinal pain, but little is known regarding the cost-effectiveness of these interventions in the U.S. Our primary objective for this project is to estimate the incremental cost-effectiveness of spinal manipulation, exercise therapy, and self-management for spinal pain using an individual patient data meta-analysis approach.
Methods/design We will estimate the incremental cost-effectiveness of spinal manipulation, exercise therapy, and self-management using cost and clinical outcome data collected in eight randomized clinical trials performed in the U.S. Cost-effectiveness will be assessed from both societal and healthcare perspectives using QALYs, pain intensity, and disability as effectiveness measures. The eight randomized clinical trials used similar methods and included different combinations of spinal manipulation, exercise therapy, or self-management for spinal pain. They also collected similar clinical outcome, healthcare utilization, and work productivity data. A two-stage approach to individual patient data meta-analysis will be conducted.
There are more articles like this @ our:
The Cost-Effectiveness of Chiropractic Page and the: