Neck Pain Patterns and Subgrouping Based on Weekly SMS-derived Trajectories
SOURCE: BMC Musculoskelet Disord 2020 (Oct 14)
P. Irgens, A. Kongsted, B. L. Myhrvold, K. Waagan, K. B. Engebretsen, B. Natvig, N. K. Vøllestad, and H. S. Robinson
Department of Interdisciplinary Health Sciences,
Institute of Health and Society,
University of Oslo, P.O. Box 1089,
Blindern, 0317, Oslo, Norway.
Background: Neck and low back pain represent dynamic conditions that change over time, often with an initial improvement after the onset of a new episode, followed by flare-ups or variations in intensity. Pain trajectories were previously defined based on longitudinal studies of temporal patterns and pain intensity of individuals with low back pain. In this study, we aimed to 1) investigate if the defined patterns and subgroups for low back pain were applicable to neck pain patients in chiropractic practice, 2) explore the robustness of the defined patterns, and 3) investigate if patients within the various patterns differ concerning characteristics and clinical findings.
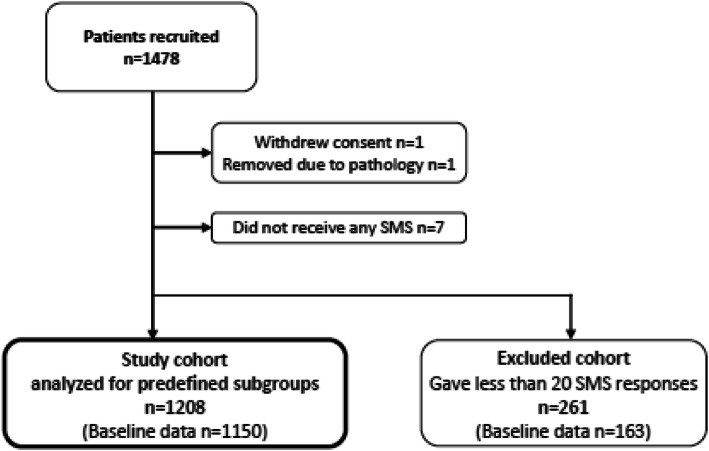
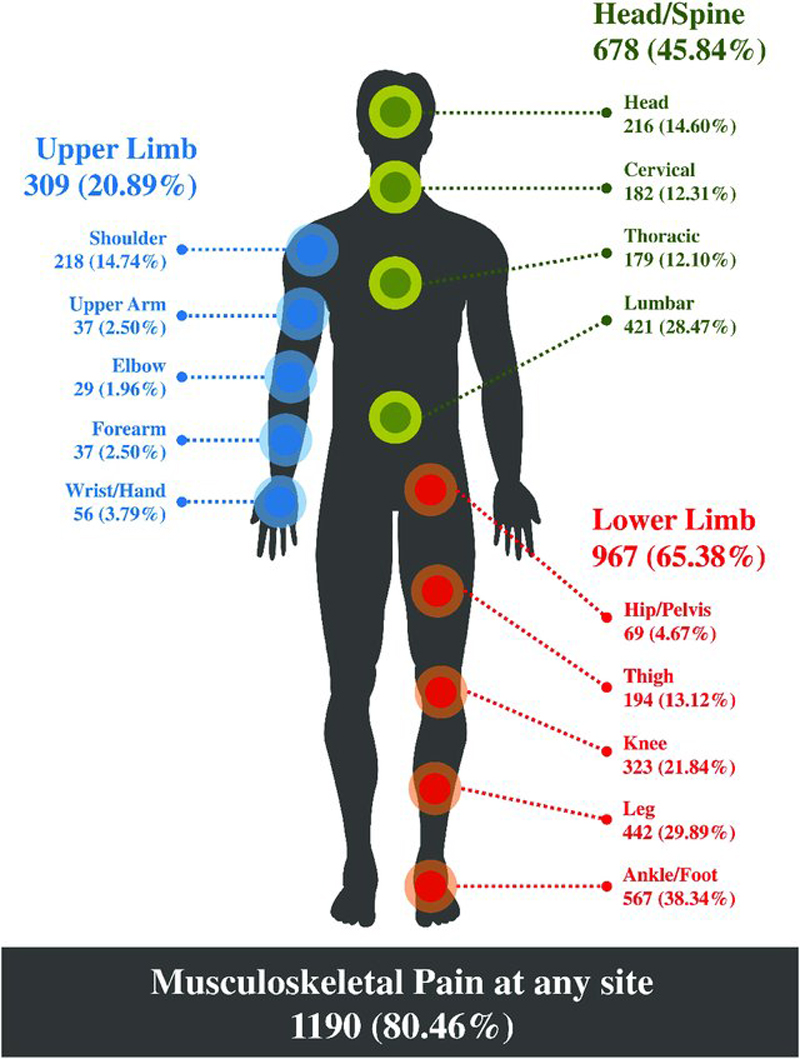
Methods: Prospective cohort study including 1208 neck pain patients from chiropractic practice. Patients responded to weekly SMS-questions about pain intensity and frequency over 43 weeks. We categorized individual responses into four main patterns based on number of days with pain and variations in pain intensity, and subdivided each into four subgroups based on pain intensity, resulting in 16 trajectory subgroups. We compared baseline characteristics and clinical findings between patterns and between Persistent fluctuating and Episodic subgroups.
Results: All but two patients could be classified into one of the 16 subgroups, with 94% in the Persistent fluctuating or Episodic patterns.
There are more articles like this @ our:
Results: All but two patients could be classified into one of the 16 subgroups, with 94% in the Persistent fluctuating or Episodic patterns. In the largest subgroup, “Mild Persistent fluctuating” (25%), mean (SD) pain intensity was 3.4 (0.6) and mean days with pain 130. Patients grouped as “Moderate Episodic” (24%) reported a mean pain intensity of 2.7 (0.6) and 39 days with pain. Eight of the 16 subgroups each contained less than 1% of the cohort. Patients in the Persistent fluctuating pattern scored higher than the other patterns in terms of reduced function and psychosocial factors.
Conclusions: The same subgroups seem to fit neck and low back pain patients, with pain that typically persists and varies in intensity or is episodic. Patients in a Persistent fluctuating pattern are more bothered by their pain than those in other patterns. The low back pain definitions can be used on patients with neck pain, but with the majority of patients classified into 8 subgroups, there seems to be a redundancy in the original model.
Keywords: Back pain; Chiropractic; Clinical course; Episodes; Fluctuations; Longitudinal; Neck pain; Subgroup.
From the FULL TEXT Article:
Background
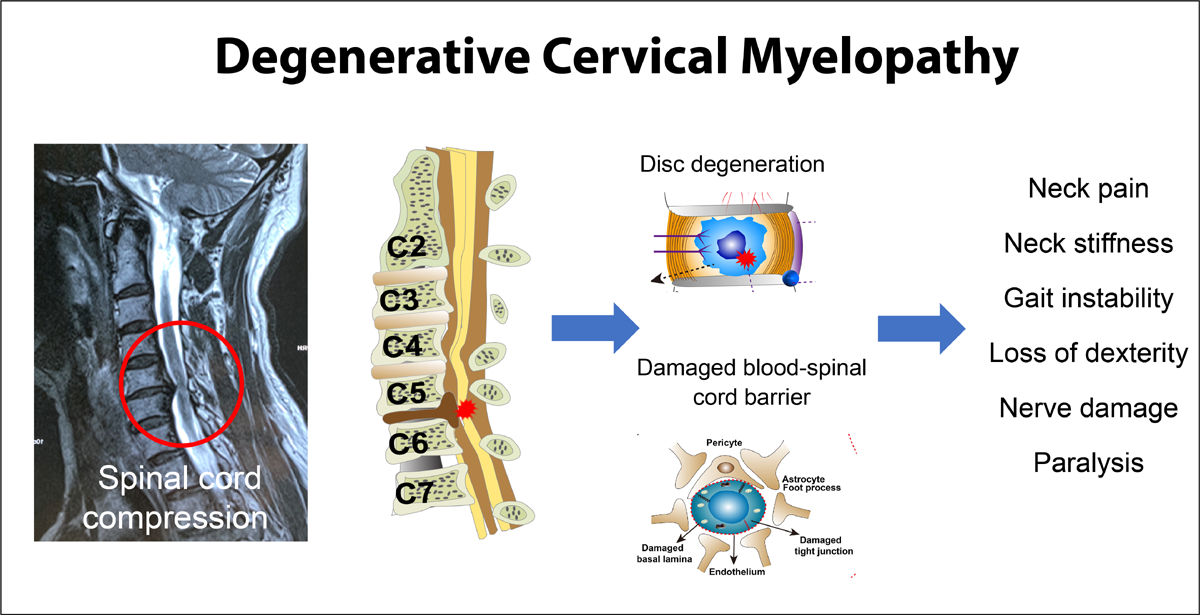
Neck pain (NP) and low back pain (LBP) are costly, common, and among the health conditions with the highest impact on disability across the world. [1] Evidence on the clinical course of spinal pain challenges the common understanding of spinal pain defined as acute, sub-acute or chronic conditions [2], and being categorized as recovered or non-recovered. [3, 4] Instead, spinal pain seems to represent dynamic conditions that change over time. In reality, the clinical course is mostly characterized by an initial improvement after the onset of a new episode, followed by flare-ups or more persistent patterns of variations in intensity or episodes. [5–8]
In a review paper, a collaborative group of LBP researchers concluded that trajectory studies on LBP are numerous and have identified similar trajectory patterns. [2] From a theoretical standpoint, it is difficult to see that future studies will uncover considerable changes in existing trajectories. However, facilitating common terminology and categorization criteria for the patterns and subgroups will help promote consistency in the field of subgroup research. Also, there is a need for assessments on the number of classes that are clinically useful and recognizable. The collaborative group advised that focus should be on subgroups constructed on a combination of pain variation patterns, pain intensity, and speed of improvement based on previously identified trajectories. [2] To further investigate the usefulness of these variation patterns, it was also recommended to test whether the findings on LBP are similar across cohorts and conditions.
Kongsted and coworkers defined 16 subgroups based on two of the suggested constructs: pain variability and pain intensity, by outlining 4 standardized definitions of variation patterns (Ongoing, Fluctuating, Episodic and Single episode). [9] These 4 patterns were further separated into 16 subgroups based on pain intensity levels (Severe, Moderate, Mild and Minor), and subsequently applied to a Danish cohort with LBP. [9] Classifications of patients using these definitions matched well with latent class analysis-derived trajectory patterns from the same cohort.
The definitions have so far only been applied to LBP patients. There are only two clinical course studies on NP for comparison. [6, 10] This limits the possibility of producing similar collaborative definitions as for LBP. However, previous studies show similarities between the clinical course of NP and LBP. [5, 6, 11] In addition, patients with NP and LBP have several similarities in psychosocial prognostic factors and comorbidities, clinical guidelines for best practice, and lack of specific pathoanatomic causality. [11–14] While the models for clinical management of musculoskeletal complaints to date have mainly been condition specific, there have recently been calls for management based on characteristics within the biopsychosocial model regardless of pain condition. [14–17] Studies have also demonstrated that patients with trajectories of NP display similar on most health-related factors as for LBP. [5, 6] Thus, as a next step in subgroup development it is important to examine how well the definitions based on LBP will fit in a NP cohort, and if the group of patients in the patterns differ with regards to clinical characteristics.
Read the rest of this Full Text article now!



Leave A Comment