The Association Between Cervical Degenerative MRI Findings and Self-reported Neck Pain, Disability and Headache: A Cross-sectional Exploratory Study
SOURCE: Chiropractic & Manual Therapies 2023 (Oct 11); 31: 45
Rikke K Jensen • Kristina B Dissing • Tue S Jensen • Stine H Clausen • Bodil Arnbak
Department of Sports Science and Clinical Biomechanics,
Center for Muscle and Joint Health,
University of Southern Denmark,
Odense, Denmark.
FROM: J. Clin. Med. 2021
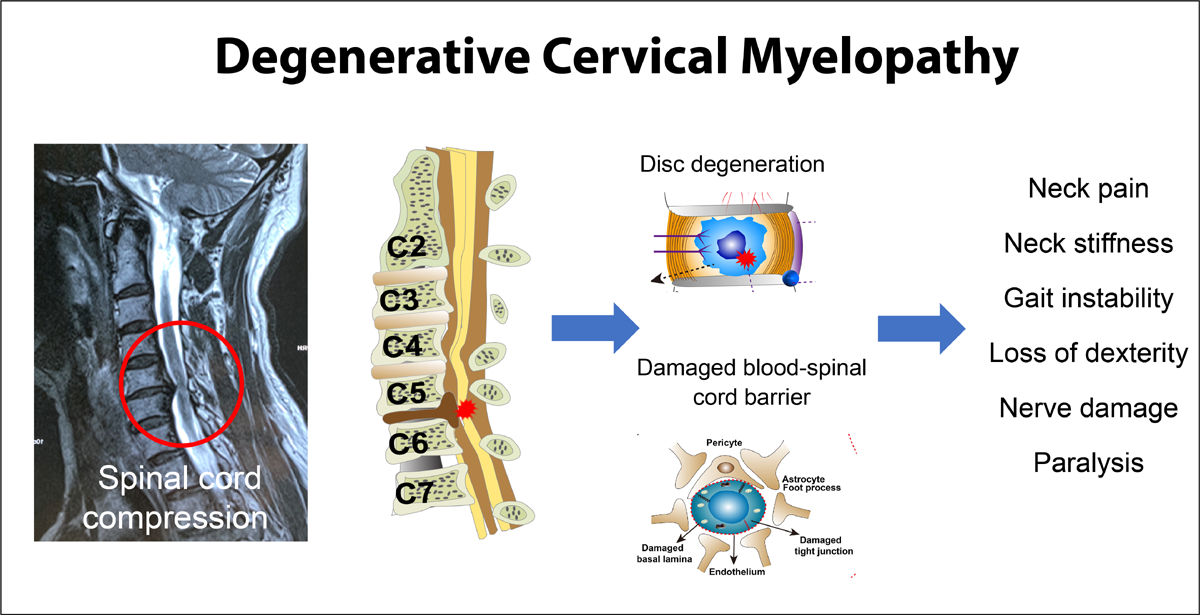
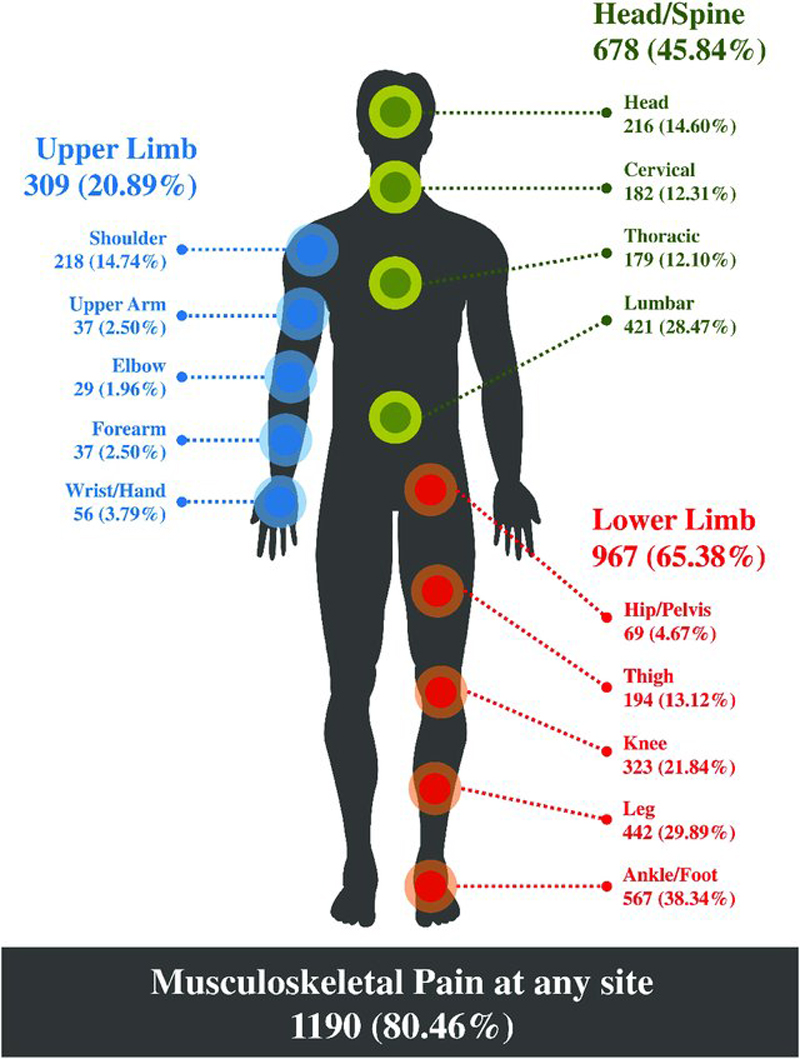
Background: Neck pain and headache are highly prevalent conditions and leading causes of disability worldwide. Although MRI is widely used in the management of these conditions, there is uncertainty about the clinical significance of cervical MRI findings in patients with neck pain or headache. Therefore, this study aims to investigate the association between cervical degenerative MRI findings and self-reported neck pain, neck disability, and headache.
Methods: This study was a secondary analysis of a cohort of patients with low back pain aged 18-40 years recruited from a non-surgical outpatient spine clinic. The cervical MRI and outcome measures used in this analysis were collected at a four-year follow-up (2014-2017). Self-reported outcome measures included neck pain intensity, neck disability as measured by the Neck Disability Index, and headache as measured by a single NDI item. Cervical MRI findings included disc degeneration, disc contour changes, and vertebral endplate signal changes (VESC). Multivariable logistic regression analyses, adjusted for age and sex, were used to analyse the associations between MRI findings and neck pain, neck disability, and headache.
There are more articles like this @ our:
Results: A total of 600 participants who underwent MRI and completed the relevant questionnaires at follow-up were included. The median age was 37 years (interquartile range 31-41) and 325 (54%) were female. Of the included participants, 181 (31%) had moderate or severe neck pain, 274 (59%) had moderate or severe neck disability, 193 (42%) reported headaches, and 211 (35%) had one or more cervical degenerative MRI findings. Cervical disc degeneration and disc contour changes were positively associated with moderate or severe neck pain with odds ratio 1.6 (95% CI 1.1-2.4) and 1.6 (1.1-2.3), respectively. VESC was associated with moderate or severe neck disability with odds ratio 3.3 (1.3-8.4). No statistically significant associations were found between the MRI findings assessed and headache.
Conclusions: In this cross-sectional exploratory study, we found that cervical disc degeneration and disc contour changes were associated with neck pain, and VESC was associated with neck disability. None of the MRI findings were associated with headache. The results suggest that cervical degenerative changes may contribute to the aetiology of neck symptoms, but the associations are modest and cannot guide clinical decisions.
Keywords: Disc contour; Disc degeneration; Headache; MRI; Neck Disability Index; Neck pain; Vertebral endplate signal changes.
From the FULL TEXT Article:
Background
Neck pain (NP) and headache are highly prevalent and leading causes of disability globally [1-3], and they often co-occur. [4, 5] Despite the socioeconomic and individual burden of NP and headache, these conditions have received far less research attention than, for example, low back pain (LBP), which shares many similarities with NP. [6]
The aetiology of NP is multifactorial, including biological, psychological, and social factors. However, evidence on the underlying pathology of NP is sparse. In most cases of NP, the specific pathological cause of symptoms cannot be identified once serious pathologies (e.g., cancer, fracture) and nerve root involvement have been ruled out. [6] Similarly, a possible relationship between headache and structural changes in the cervical spine remains unclear. [7, 8] Therefore, research that contributes to understanding the aetiology of NP and headache is warranted.
Magnetic resonance imaging (MRI) has the potential to identify anatomical structures that may contribute to a patient’s pain or disability and is commonly used in the clinical evaluation of patients with NP. [9] Changes such as disc degeneration, disc herniation, and vertebral endplate signal changes (VESC) can be visualised by MRI. However, the clinical relevance of MRI-defined structural spinal changes remains controversial, mainly because degenerative MRI changes are often observed in asymptomatic individuals. Furthermore, the association with treatment response in clinical populations and the association with pain in the general population have not been thoroughly investigated. [10, 11]
In patients with LBP, positive associations between some MRI findings (e.g., disc contour, disc degeneration, Modic changes type 1 (VESC with bone marrow oedema)) and pain are consistent at a population level. [12] A similar association may exist for NP. However, few studies have investigated the association between cervical MRI findings and NP. [13, 14] Similarly, there are very few studies on the association between headache and cervical MRI findings, and the evidence is inconclusive. [8, 15]
The Spines of Southern Denmark (SSD) cohort was initiated to evaluate the association between LBP, spondyloarthritis and MRI findings in patients with persistent LBP referred to a regional secondary care spine centre. MRI and survey information on NP, neck disability and headache were collected as part of the four-year follow-up of the cohort. This exploratory secondary analysis of the cohort aims to investigate the association between cervical degenerative MRI findings and self-reported NP, neck disability, and headache.




Leave A Comment