Access to Chiropractic Care and the Cost of Spine Conditions Among Older Adults
SOURCE: American J Managed Care 2019 (Aug); 25 (8): e230–e236
Matthew A. Davis, PhD, DC, MPH et. al.
Matthew A. Davis, PhD, DC, MPH
University of Michigan,
400 N Ingalls St, Room 4347,
Ann Arbor, MI 48109.
Objectives: Chiropractic care is a service that operates outside of the conventional medical system and is reimbursed by Medicare. Our objective was to examine the extent to which accessibility of chiropractic care affects spending on medical spine care among Medicare beneficiaries.
Study Design: Retrospective cohort study that used beneficiary relocation as a quasi-experiment.
Methods: We used a combination of national data on provider location and Medicare claims to perform a quasi-experimental study to examine the effect of chiropractic care accessibility on healthcare spending. We identified 84,679 older adults enrolled in Medicare with a spine condition who relocated once between 2010 and 2014. For each year, we measured accessibility using the variable-distance enhanced 2-step floating catchment area method. Using data for the years before and after relocation, we estimated the effect of moving to an area of lower or higher chiropractic accessibility on spine-related spending adjusted for access to medical physicians.
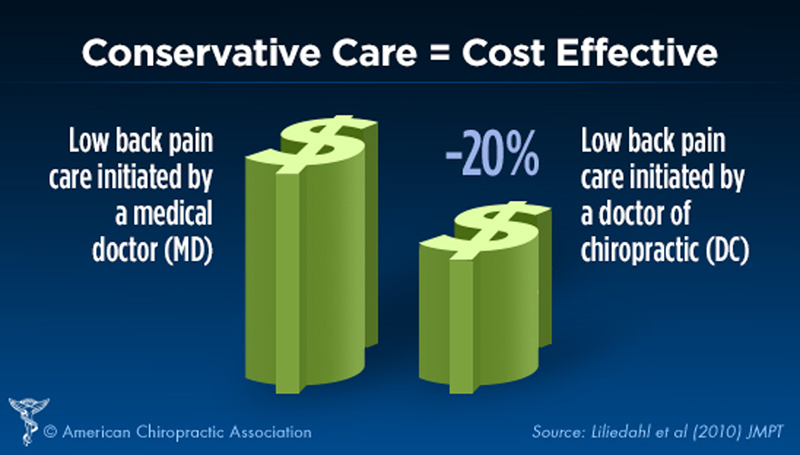
Results: There are approximately 45,000 active chiropractors in the United States, and local accessibility varies considerably. A negative dose–response relationship was observed for spine-related spending on medical evaluation and management as well as diagnostic imaging and testing (mean differences, $20 and $40, respectively, among those exposed to increasingly higher chiropractic accessibility; P <.05 for both). Associations with other types of spine-related spending were not significant.
There are more articles like this @ our:
Conclusions: Among older adults, access to chiropractic care may reduce medical spending on services for spine conditions.
From the FULL TEXT Article:
Background
Back pain and neck pain are associated with an estimated direct cost of $86 billion to the United States economy. [1] Among the top contributors to disability, back pain and neck pain outrank chronic diseases such as chronic pulmonary disease, ischemic heart disease, and diabetes. [2] Although back pain can be attributed to a serious underlying medical problem, up to 85% of cases are classified as nonspecific (ie, cases without an underlying pathology). [3] Approximately one-fourth of all adults will experience nonspecific back pain during a 3–month period, and at any one point in time, approximately 30% of older adults suffer from back pain. [4] Older adults are particularly vulnerable to back pain and most who experience nonspecific back pain have future recurrences [4, 5]; thus, it is among the most common reasons older Americans visit physicians. [6]
With more than 100 million visits for spine conditions each year, [7, 8] the chiropractic profession is the largest health service that operates outside of the conventional medical system [9, 10] and the only such service reimbursed by Medicare. [11, 12] Medicare beneficiaries can use chiropractic care without a medical referral; however, the only reimbursable modality is manual therapy, which costs approximately $30 to $50 per visit. Chiropractors cannot be reimbursed directly for diagnostic imaging nor prescribe medications. In light of the ongoing debate regarding coverage of presumably nonessential services, there is a specific need to more rigorously examine how chiropractic care may affect national healthcare spending.
Previous observational research that has examined spending among chiropractic patients compared with medical care patients suggests that chiropractic care may reduce utilization of and expenditures on medical services for back pain. [13, 14] Traditional observational studies use assignment of patients to a specific treatment type (eg, chiropractic vs usual care) to study the cost of chiropractic care. These designs, however, are unable to account for the potential impacts from those who choose to use chiropractic care in place of medical care. To date, previous studies have neglected to consider such indirect effects of the service on the system at large.
Therefore, we performed a quasi-experimental study to examine how accessibility of chiropractic care among Medicare beneficiaries affects healthcare spending for spine conditions. To do so, we used a cohort of older adults in Medicare with back and/or neck pain who relocated and experienced a change in geographic accessibility of chiropractic care. In this way, the change in accessibility of chiropractic care served as a proxy for access to the service among Medicare beneficiaries, providing us with the unique opportunity to observe how either reducing or increasing access affects spine-related spending among older adults.



Leave A Comment