Spinal Manipulation and Exercise for Low Back Pain in Adolescents: A Randomized Trial
SOURCE: Pain. 2018 (Jul); 159 (7): 1297–1307
Roni Evans, Mitchell Haas, Craig Schulz, Brent Leininger, Linda Hanson, and Gert Bronfort
Integrative Health & Wellbeing Research Program,
Earl E. Bakken Center for Spirituality and Healing,
University of Minnesota,
Minneapolis, MN, USA.
Low back pain (LBP) is common in adolescence, but there is a paucity of high-quality research to inform care. We conducted a multicenter randomized trial comparing 12 weeks of spinal manipulative therapy (SMT) combined with exercise therapy (ET) to ET alone.
Participants were 185 adolescents aged 12 to 18 years with chronic LBP.
The primary outcome was LBP severity at 12, 26, and 52 weeks. Secondary outcomes included disability, quality of life, medication use, patient- and caregiver-rated improvement, and satisfaction. Outcomes were analyzed using longitudinal linear mixed effect models. An omnibus test assessing differences in individual outcomes over the entire year controlled for multiplicity.
Of the 185 enrolled patients, 179 (97%) provided data at 12 weeks and 174 (94%) at 26 and 52 weeks. Adding SMT to ET resulted in a larger reduction in LBP severity over the course of 1 year (P = 0.007). The group difference in LBP severity (0–10 scale) was small at the end of treatment (mean difference = 0.5; P = 0.08) but was larger at weeks 26 (mean difference = 1.1; P = 0.001) and 52 (mean difference = 0.8; P = 0.009). At 26 weeks, SMT with ET performed better than ET alone for disability (P = 0.04) and improvement (P = 0.02). The SMT with ET group reported significantly greater satisfaction with care at all time points (P ≤ 0.02). There were no serious treatment-related adverse events.
There are more articles like this @ our:
For adolescents with chronic LBP, spinal manipulation combined with exercise was more effective than exercise alone over a 1–year period, with the largest differences occurring at 6 months. These findings warrant replication and evaluation of cost effectiveness.
ClinicalTrials.gov Identifier: NCT01096628
From the Full-Text Article:
Introduction
The United States is in the midst of an unprecedented pain management crisis, with chronic pain impacting over ⅓ of the US population, and affecting more individuals than heart disease, diabetes, and cancer combined. [43] LBP is one of the most common and burdensome of the pain conditions with an estimated 40–80% of individuals worldwide experiencing LBP at some point in their lives. [25, 31] LBP related disability has increased an alarming 42% over the past two decades, making it the leading cause of disability globally. [32] While there has been a long-standing belief that LBP is limited to adults, there is now substantial evidence to the contrary. In fact, research has shown that LBP develops with increasing frequency in adolescence, with prevalence rates reaching that of adults by the late teens. [10, 33, 34, 37] Importantly, adolescent LBP has been shown to be a strong predictor of adult LBP, which may have important negative implications for the lifetime course. [17, 28, 33] An additional concern is that 20%–40% of U.S. adolescent LBP sufferers receive an opioid prescription when they seek medical care. [24, 51] There is a heightened urgency to identify safe and effective nonpharmacological
LBP treatments for all ages. [12]
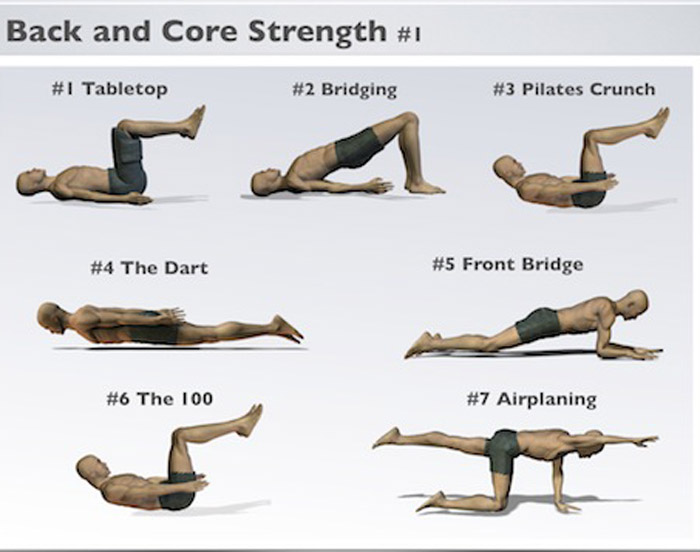
In 2012, complementary healthcare approaches were used by one third of American adults [13] and 12% of children 4–17. [4] Spinal manipulative therapy (SMT) is the most common provider based complementary approach [4, 13] and is often used to treat LBP complaints. SMT consists of manual techniques including high velocity, low amplitude thrust procedures or low velocity, variable amplitude mobilization maneuvers. For LBP, SMT is applied to the lumbar vertebral or sacroiliac joints with the aim of restoring mobility and decreasing pain. [26] Recent guidelines for LBP in adults strongly recommended SMT as well as exercise prior to initiating pharmacologic treatment. [50] Rehabilitative exercise focused on teaching and encouraging patients how to manage their LBP, and potentially prevent future recurrences, is frequently combined with SMT as an important aspect of promoting patient self-efficacy. [15]
While there is fairly well established evidence regarding the effectiveness of commonly used conservative treatments like supervised exercise and SMT for adults with chronic LBP, [12, 52] there are few randomized trials focusing on adolescents with LBP. [10, 44] Indeed, a systematic review of conservative treatments for LBP in children and adolescents was unable to locate any trials focused on SMT, and only three small studies [1, 20, 35] focused on exercise. Thus there is a critical need for more high quality RCTs to inform the responsible management of LBP in non-adult populations. [44]
To address the large research gaps for LBP management in adolescents, we performed a parallel-group, randomized controlled trial to test the comparative effectiveness of SMT plus exercise therapy (ET) versus ET alone for individuals 12–18 years of age with recurrent or chronic LBP. We chose exercise alone as a comparison intervention because of the encouraging preliminary evidence of effectiveness for adolescents with LBP and the potential to promote active pain coping behaviors.[44] The primary aim of this study was to test the hypothesis that the addition of SMT to exercise would be more effective than exercise alone at 12, 26, and 52 weeks in improving LBP pain severity. The impact on other important LBP related outcomes, including disability, quality of life, medication use, patient and caregiver-rated improvement and satisfaction, was also assessed.
Read the rest of this Full Text article now!



Leave A Comment