Association Between Centralization and Directional Preference and Functional and Pain Outcomes in Patients With Neck Pain
SOURCE: J Orthop Sports Phys Ther. 2014 (Feb); 44 (2): 68–75
Susan L. Edmond, PT, DSc, OCS, Guillermo Cutrone, PT, DSc, OCS, Cert MDT, FAAOMPT, Mark Werneke, PT, MS, Dip MDT et. al.
Rutgers,
The State University of New Jersey,
Newark, NJ.
STUDY DESIGN: Retrospective cohort.
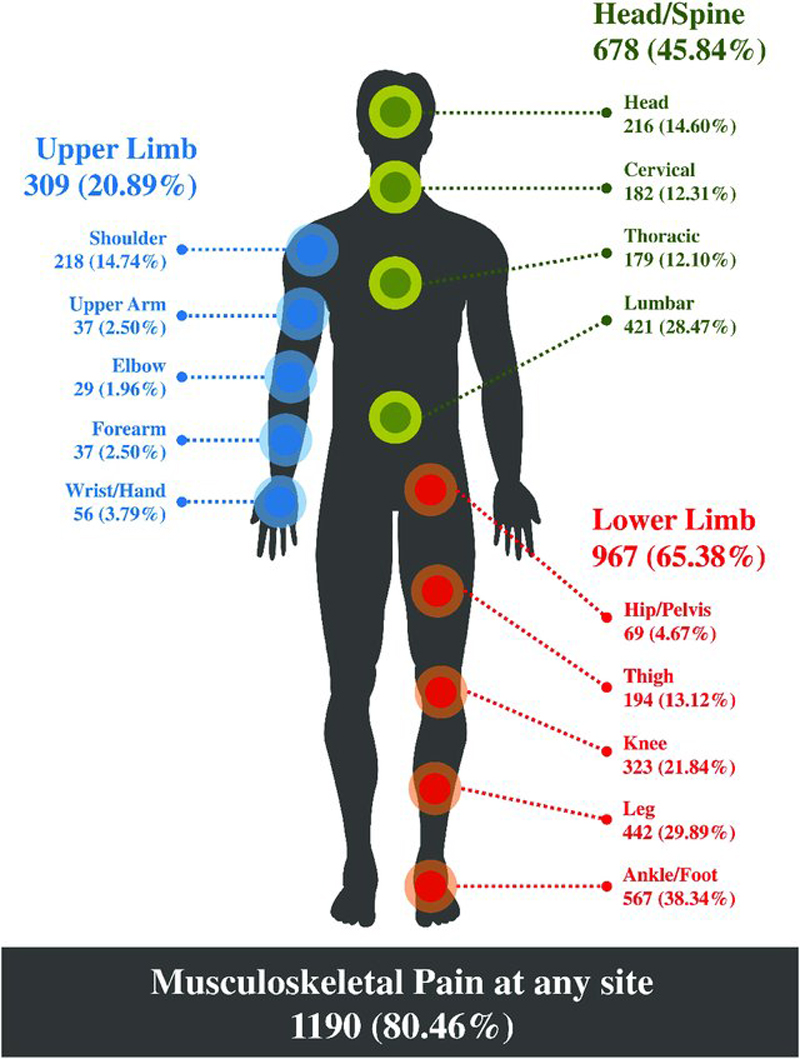
OBJECTIVES: In subjects with neck pain, the present study aimed (1) to describe the prevalence of centralization (CEN), noncentralization (non-CEN), directional preference (DP), and no directional preference (no DP); (2) to determine if age, sex, fear-avoidance beliefs about physical activity, number of comorbid conditions, or symptom duration varies among subjects who demonstrate CEN versus non-CEN and DP versus no DP; and (3) to determine if CEN and/or DP are associated with changes in function and pain.
BACKGROUND: CEN and DP are prevalent among patients with low back pain and should be considered when determining treatment strategies and predicting outcomes; however, these findings are not well investigated in patients with neck pain.
METHODS: Three hundred four subjects contributed data. CEN and DP prevalence were calculated, as was the association between CEN and DP, and age, sex, number of comorbid conditions, fear-avoidance beliefs, and symptom duration. Multivariate models assessed whether CEN and DP predicted change in function and pain.
RESULTS: CEN and DP prevalence were 0.4 and 0.7, respectively. Younger subjects and those with fewer comorbid conditions were more likely to centralize; however, subjects who demonstrated DP were more likely to have acute symptoms. Subjects who centralized experienced, on average, a 3.6-point (95% confidence interval: -0.3, 7.4) improvement in function scores, whereas subjects with a DP averaged a 5.4-point (95% confidence interval: 0.8, 10.0) improvement. Neither CEN nor DP was associated with pain outcomes.
There are more articles like this @ our:
CONCLUSION: directional preference (DP) and, to a lesser extent, centralization (CEN) represent evaluation categories that are associated with improvements in functional outcomes.
From the FULL TEXT Article:
Introduction
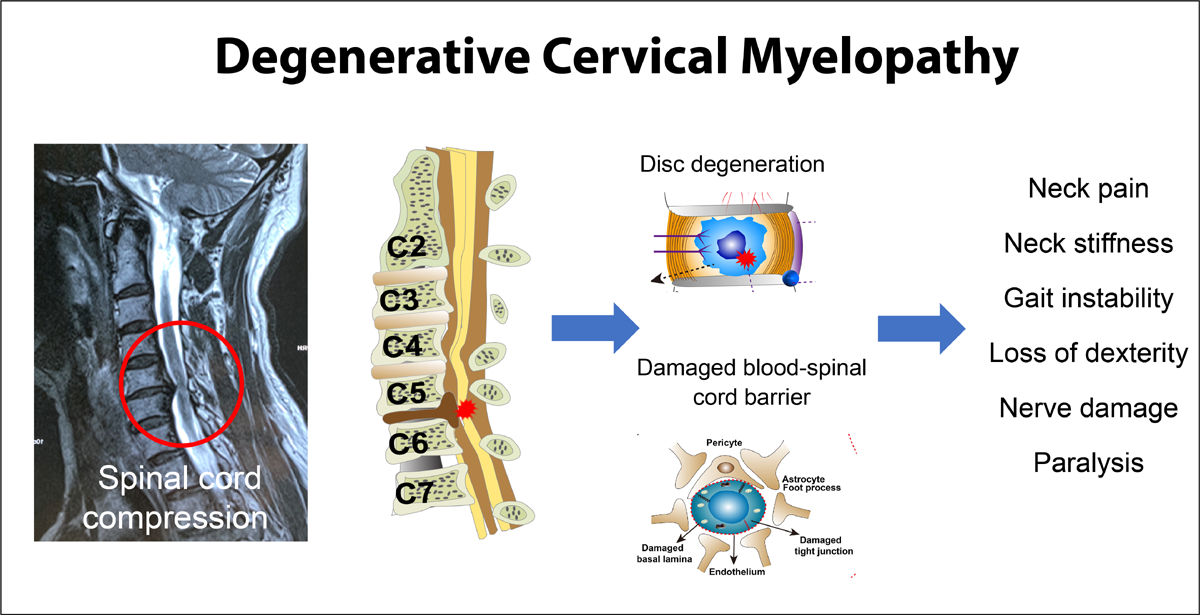
Researchers have suggested that classifying patients into subgroups based on clinical characteristics and matching these subgroups to management strategies improve patient outcomes of physical therapy interventions. [5, 10, 26, 37] Classification of patients with neck pain has been recommended as a research priority. [5, 16] Nevertheless, there is insufficient information regarding how to classify these patients to inform physical therapy interventions that optimize outcomes.
Two examination procedures used to classify patients with spinal pain have been studied: centralization (CEN) and directional preference (DP). These examination procedures, which are derived from Mechanical Diagnosis and Therapy methods, inform clinical decisions and guide patient management. A classification method that combines CEN and DP principles, called the “patient response method,” has subsequently been proposed and recommended for use with patients with nonserious lumbar spine pain. [36]
A number of studies have demonstrated that in relation to low back pain, CEN and DP are of clinical value. CEN has been shown to predict decreased disability, [9, 28, 32-34, 37] return to work, [17, 23, 32, 35] and reduced pain. [9, 23, 32-34, 37] In several studies, prescribing exercises matched to the patient’s DP has improved low back pain outcomes. [2, 20-23] In 1 study (level 3 evidence), [8] the authors suggested that the patient response method delineated and improved the prediction of pain and function outcomes in patients with low back pain. [36]
CEN is operationally defined as spinal pain that is progressively abolished in a distal-to-proximal direction in response to therapeutic movement and positioning strategies, without consideration of intensity. [24, 26, 34, 37] DP is determined by whether spine and/or referred spinal pain located in the most distal body part decreases in intensity, abolishes, or centralizes, and/or whether subjects demonstrate an improvement in range of motion in response to a repeated-movement or positional-loading strategy. [25] Individuals not meeting these criteria are considered to have non-CEN and no DP, respectively.
The decision rules for judging CEN and DP are therefore similar but not synonymous. When CEN is present, DP must also be present. In contrast, DP might occur in the absence of CEN (eg, a patient’s lower-leg pain may decrease in intensity but not change in location with a specific repeated-movement or positional-loading strategy). CEN has also been shown to occur in the cervical spine. The prevalence of CEN, identified using the same operational definition described above, was reported to be 0.3, [24] 0.4, [6] and 0.2 [37] in prior studies. In the latter study, [37] prevalence decreased among more chronic and older subjects. The prevalence of DP among subjects with neck pain has not been reported in prior literature and remains unknown.
SOURCE: Read the rest of this Full Text article now!




Leave A Comment