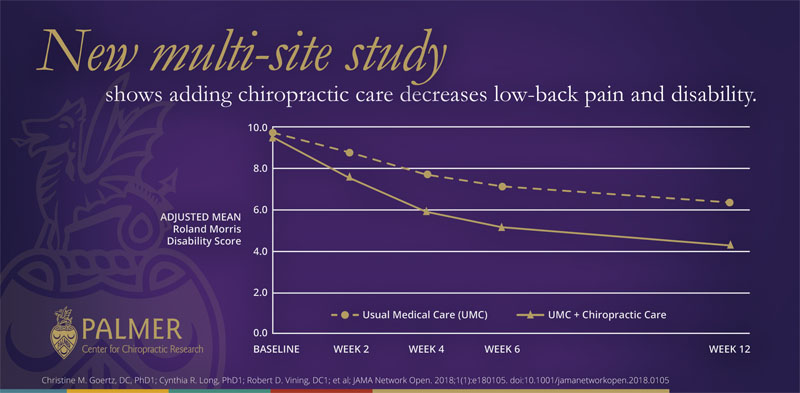
Effect of Usual Medical Care Plus Chiropractic Care vs Usual Medical Care Alone
on Pain and Disability Among US Service Members With Low Back Pain.
A Comparative Effectiveness Clinical Trial
SOURCE: JAMA Network Open. 2018 (May 18); 1 (1): e180105
Christine M. Goertz, DC, PhD 1; Cynthia R. Long, PhD 1; Robert D. Vining, DC 1; Katherine A. Pohlman, DC, MS 2; Joan Walter, JD, PA 3; Ian Coulter, PhD 4
(1) Palmer College of Chiropractic,
Palmer Center for Chiropractic Research,
Davenport, Iowa
(2) Parker University Research Institute,
Dallas, Texas
(3) Samueli Institute for Information Biology,
Silver Spring, Maryland
(4) RAND Corporation,
Santa Monica, California
Importance It is critically important to evaluate the effect of nonpharmacological treatments on low back pain and associated disability.
Objective To determine whether the addition of chiropractic care to usual medical care results in better pain relief and pain-related function when compared with usual medical care alone.
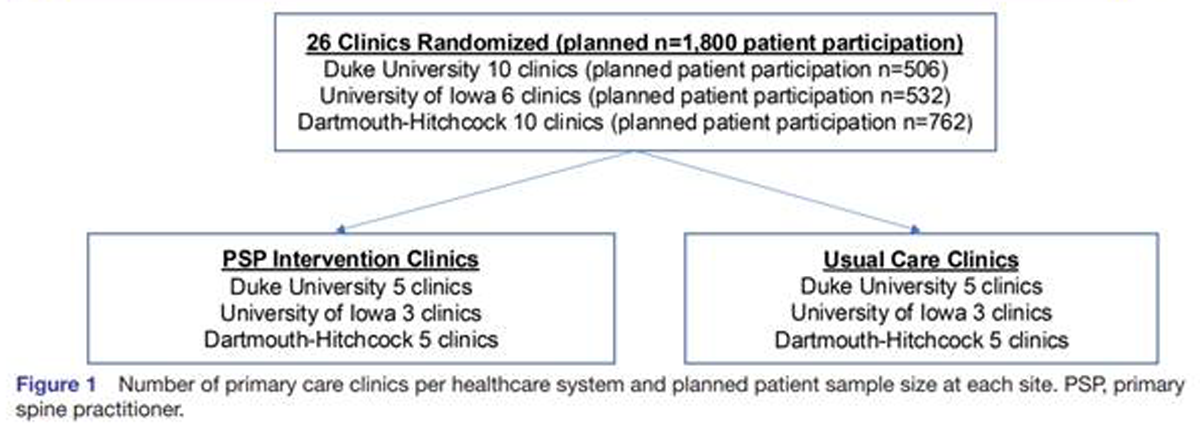
Design, Setting, and Participants A 3–site pragmatic comparative effectiveness clinical trial using adaptive allocation was conducted from September 28, 2012, to February 13, 2016, at 2 large military medical centers in major metropolitan areas and 1 smaller hospital at a military training site. Eligible participants were active-duty US service members aged 18 to 50 years with low back pain from a musculoskeletal source.
Interventions The intervention period was 6 weeks. Usual medical care included self-care, medications, physical therapy, and pain clinic referral. Chiropractic care included spinal manipulative therapy in the low back and adjacent regions and additional therapeutic procedures such as rehabilitative exercise, cryotherapy, superficial heat, and other manual therapies.
Main Outcomes and Measures Coprimary outcomes were low back pain intensity (Numerical Rating Scale; scores ranging from 0 [no low back pain] to 10 [worst possible low back pain]) and disability (Roland Morris Disability Questionnaire; scores ranging from 0–24, with higher scores indicating greater disability) at 6 weeks. Secondary outcomes included perceived improvement, satisfaction (Numerical Rating Scale; scores ranging from 0 [not at all satisfied] to 10 [extremely satisfied]), and medication use. The coprimary outcomes were modeled with linear mixed-effects regression over baseline and weeks 2, 4, 6, and 12.
Results Of the 806 screened patients who were recruited through either clinician referrals or self-referrals, 750 were enrolled (250 at each site). The mean (SD) participant age was 30.9 (8.7) years, 175 participants (23.3%) were female, and 243 participants (32.4%) were nonwhite. Statistically significant site × time × group interactions were found in all models. Adjusted mean differences in scores at week 6 were statistically significant in favor of usual medical care plus chiropractic care compared with usual medical care alone overall for low back pain intensity (mean difference, –1.1; 95% CI, –1.4 to –0.7), disability (mean difference, –2.2; 95% CI, –3.1 to –1.2), and satisfaction (mean difference, 2.5; 95% CI, 2.1 to 2.8) as well as at each site. Adjusted odd ratios at week 6 were also statistically significant in favor of usual medical care plus chiropractic care overall for perceived improvement (odds ratio = 0.18; 95% CI, 0.13–0.25) and self-reported pain medication use (odds ratio = 0.73; 95% CI, 0.54–0.97). No serious related adverse events were reported.
There are more articles like this @ our:
Chiropractic Care For Veterans Page and the:
Conclusions and Relevance Chiropractic care, when added to usual medical care, resulted in moderate short-term improvements in low back pain intensity and disability in active-duty military personnel. This trial provides additional support for the inclusion of chiropractic care as a component of multidisciplinary health care for low back pain, as currently recommended in existing guidelines. However, study limitations illustrate that further research is needed to understand longer-term outcomes as well as how patient heterogeneity and intervention variations affect patient responses to chiropractic care.
Trial Registration ClinicalTrials.gov Identifier: NCT01692275
You will also enjoy this Medscape Medical News review of this study, titled:
Chiropractic Care Improves Usual Management for Low Back Pain
and this comment by the chief author, from an interview with: MedicalResearch.com
|
This patient-centered, multi-site, pragmatic clinical trial study provides the strongest evidence to-date that chiropractic care is safe, effective and can be integrated into multidisciplinary healthcare settings. These findings are important as the United States health-care system looks for ways to implement existing national guidelines from groups such as the American College of Physicians and the Joint Commission that recommend non-drug treatments, such as spinal manipulative therapy, as the first line of treatment for low-back pain. |
From the FULL TEXT Article:
| Key Points Question What is the effect of adding chiropractic care to usual medical care for patients with low back pain?
Findings In this comparative effectiveness clinical trial among active-duty US military personnel, patients who received usual medical care plus chiropractic care reported a statistically significant moderate improvement in low back pain intensity and disability at 6 weeks compared with those who received usual care alone. Meaning This trial supports the inclusion of chiropractic care as a component of multidisciplinary health care for low back pain, as currently recommended in existing guidelines. |
Introduction
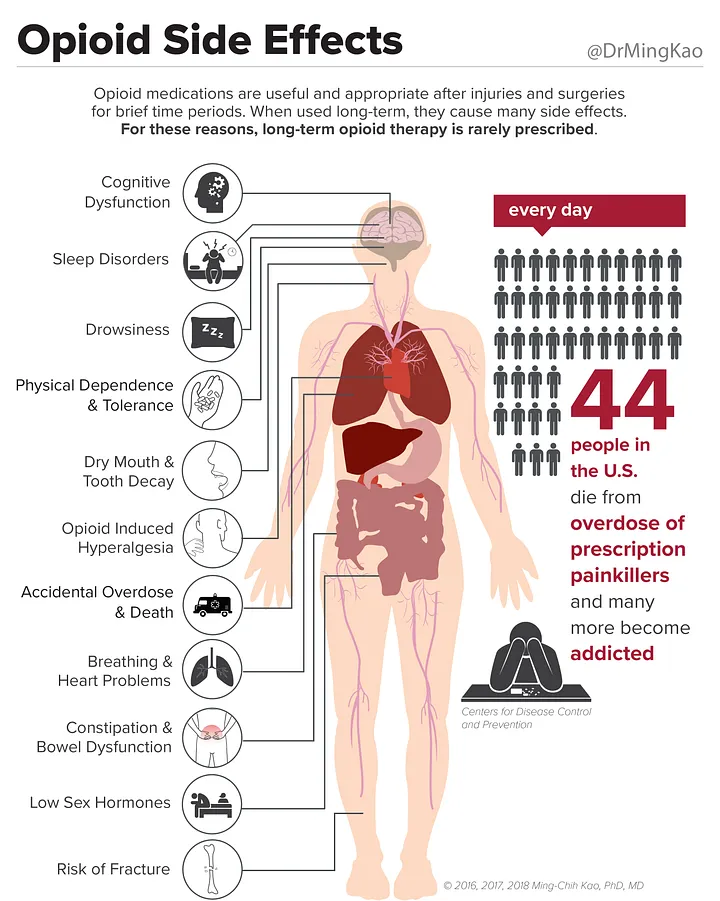
Musculoskeletal disorders are the second leading cause of disability worldwide, led by low back pain (LBP), with an estimated LBP prevalence among US adults of 20%. [1–3] The direct costs of back pain in the United States in 2010 were $34 billion, [4] with additional indirect costs including lost workplace productivity estimated at $200 billion. [5] In the US military, LBP is one of the most common reasons members seek medical care6 and one of the most likely conditions to interrupt combat duty. [6, 7] Common medical therapies for LBP, including nonsteroidal anti-inflammatory drugs, opioids, spinal fusions, and epidural steroid injections, demonstrate limited effectiveness [8–10]; furthermore, many of these treatments have unacceptably high risk profiles. [8, 11–14]
The US opioid crisis [15, 16] creates an urgent need to evaluate cost-effective and low-risk nonpharmacological treatments. One option is chiropractic care. Doctors of chiropractic provide conservative care focused on diagnosis, treatment, comanagement, or referral for musculoskeletal conditions, including LBP. [17] The primary therapeutic procedure used by doctors of chiropractic is spinal manipulative therapy. [18]
The use of chiropractic care is common, with annual rates among US adults estimated between 8% and 14%. [19, 20] Current guidelines recommend the use of spinal manipulative therapy and/or chiropractic care for LBP. [21, 22] Although a previous pilot study of chiropractic care for active-duty US military patients with acute LBP showed promise, [23] and chiropractic care is available at 66 military health treatment facilities worldwide, [24] significant gaps in knowledge remain in military populations. These populations tend to be younger and more diverse in terms of race and ethnicity than those included in previous trials on spinal manipulation. [25] This multisite, pragmatic clinical trial begins to address these gaps by investigating whether adding chiropractic care to usual medical care (UMC) improves outcomes for patients with LBP at military treatment facilities.
Read the rest of this Full Text article now!




Leave A Comment