Advancements in the Management of Spine Disorders
SOURCE: Best Pract Res Clin Rheumatol. 2012 (Apr); 26 (2): 263–280
Scott Haldeman, MD, Professor, Deborah Kopansky-Giles, DC, MSc, Eric L. Hurwitz, DC, PhD, Damian Hoy, BAppSc (Physio), MPH, PhD, W. Mark Erwin, DC, PhD, Simon Dagenais, DC, PhD, MSc, Greg Kawchuk, DC, PhD, Björn Strömqvist, MD, PhD, Nicolas Walsh, MD
Department of Neurology,
University of California,
Irvine, USA.

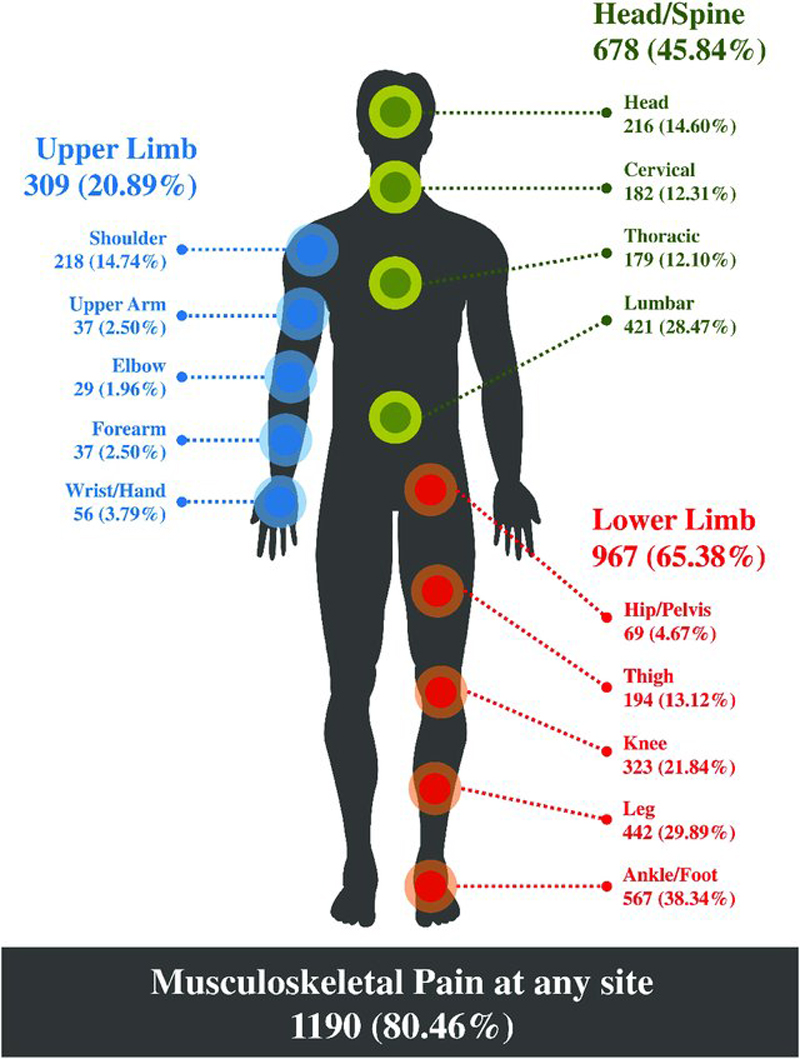
Spinal disorders and especially back and neck pain affect more people and have greater impact on work capacity and health-care costs than any other musculoskeletal condition. One of the difficulties in reducing the burden of spinal disorders is the wide and heterogeneous range of specific diseases and non-specific musculoskeletal disorders that can involve the spinal column, most of which manifest as pain. Despite, or perhaps because of its impact, spinal disorders remain one of the most controversial and difficult conditions for clinicians, patients and policymakers to manage. This paper provides a brief summary of advances in the understanding of back and neck pain over the past decade as evidenced in the current literature. This paper includes the following sections: a classification of spinal disorders; the epidemiology of spine pain in the developed and developing world; key advancements in biological and biomechanical sciences in spine pain; the current status of potential methods for the prevention of back and neck pain; rheumatological and systemic disorders that impact the spine; and evidence-based surgical and non-surgical management of spine pain.
The final section of this paper looks to the future and proposes actions and strategies that may be considered by the international Bone and Joint Decade (BJD), by providers, institutions and by policymakers so that we may better address the burden of spine disorders at global and local levels.
From the FULL TEXT Article:
Introduction
Spinal pain and its associated disorders affect more people and have greater impact on work capacity and health-care costs than any other musculoskeletal condition. Recent studies suggest that, in many societies, spinal disorders are a greater source of disability and impact the consumption of more health-care resources than any other class of diseases or health problems. [1] Despite, or perhaps because of its impact, spinal disorders remain one of the most controversial and difficult conditions for clinicians, patients and policymakers to manage.
One of the difficulties in reducing the impact of spinal pain is the wide and heterogeneous range of specific diseases and non-specific musculoskeletal disorders that can involve the spinal column, most of which manifest as spinal pain. These disorders have been classified in multiple ways but the most widely accepted classification includes four well-defined clinical categories as noted in Table 1.
There are more articles like this @ our:
- Spinal disorders with serious or systemic pathology. This category includes disorders caused by congenital and developmental abnormalities, neoplasm, infection disorders, systemic inflammatory disorders and serious trauma. It has been reported that serious spinal pathology, however, accounts for only 1–2% of patients who present with symptoms of spinal pain. [2, 3]
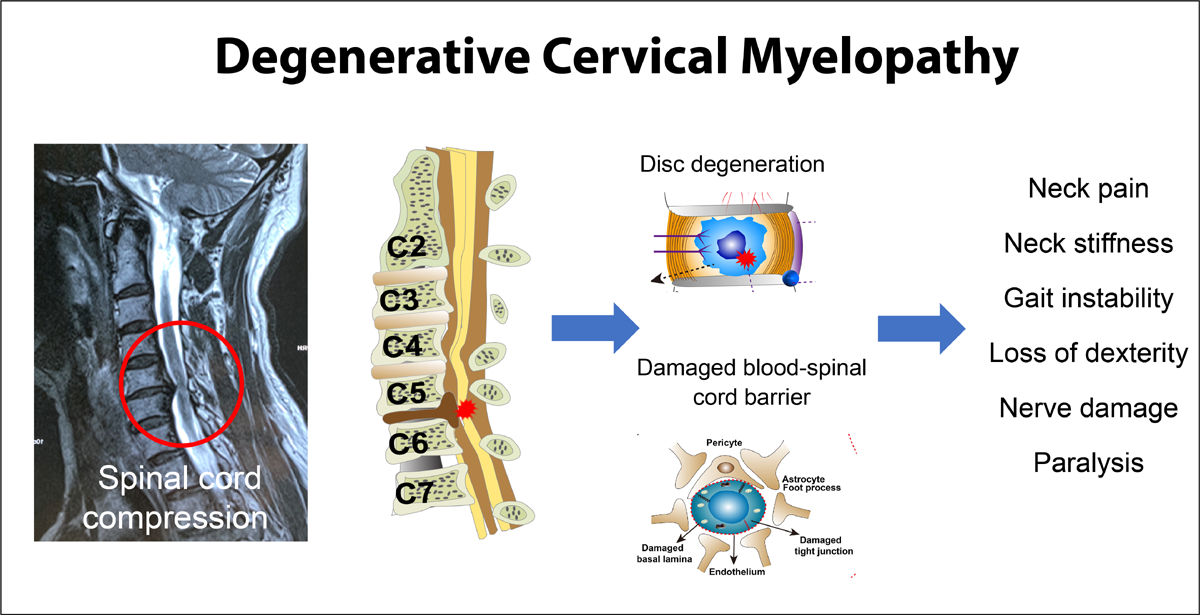
- Spinal pain with neurological deficits. The primary neurological deficits that fall into this category include compression of nerve roots, the spinal cord or the cauda equina. It has been estimated that 5–10% of patients presenting with low back pain (LBP) have substantial neurologic involvement. [3] In one survey, features of sciatica were reported by 11.6% of those with LBP; unfortunately, this study did not determine the frequency of actual neurological deficits which is estimated to be a considerably smaller percentage. [4] A recent 10-year survey from the US military noted an incidence of cervical radiculopathy at 1.79 per 1000 person-years. [5]
- Non-specific spinal pain, which has also been described as mechanical pain or strain accounts for 90% or more of all people who experience spinal pain. There is growing evidence that it is not currently possible to identify the structure, pathology or source of pain in the majority of patients with these symptoms. Clinicians have postulated that pain can be generated by virtually all tissues of the spine and have defined pain syndromes based on the specific tissues, structures or suspected pathology which are assumed to be causing pain. These theories, however, have yet to be widely accepted and many of the testing methods for these suspected diagnoses have yet to be validated.
- Spinal pain referred from non-spinal pathology. A number of systemic, abdominal and pelvic pathologies may present as spinal pain. There are no data to determine how frequently this type of referred pain occurs but it is commonly included as a symptom of a number of visceral disorders as listed in Table 1.
Read the rest of this Full Text article now!



Leave A Comment