Provider and Patient Perspectives on Opioids and Alternative Treatments for Managing Chronic Pain:
A Qualitative Study
SOURCE: BMC Fam Pract. 2017 (Mar 24); 17 (1): 164
Lauren S. Penney, Cheryl Ritenbaugh, Lynn L. DeBar,
Charles Elder and Richard A. Deyo
South Texas Veterans Health Care System,
7400 Merton Minter Blvd,
San Antonio, TX, 78229, USA
BACKGROUND: Current literature describes the limits and pitfalls of using opioid pharmacotherapy for chronic pain and the importance of identifying alternatives. The objective of this study was to identify the practical issues patients and providers face when accessing alternatives to opioids, and how multiple parties view these issues.
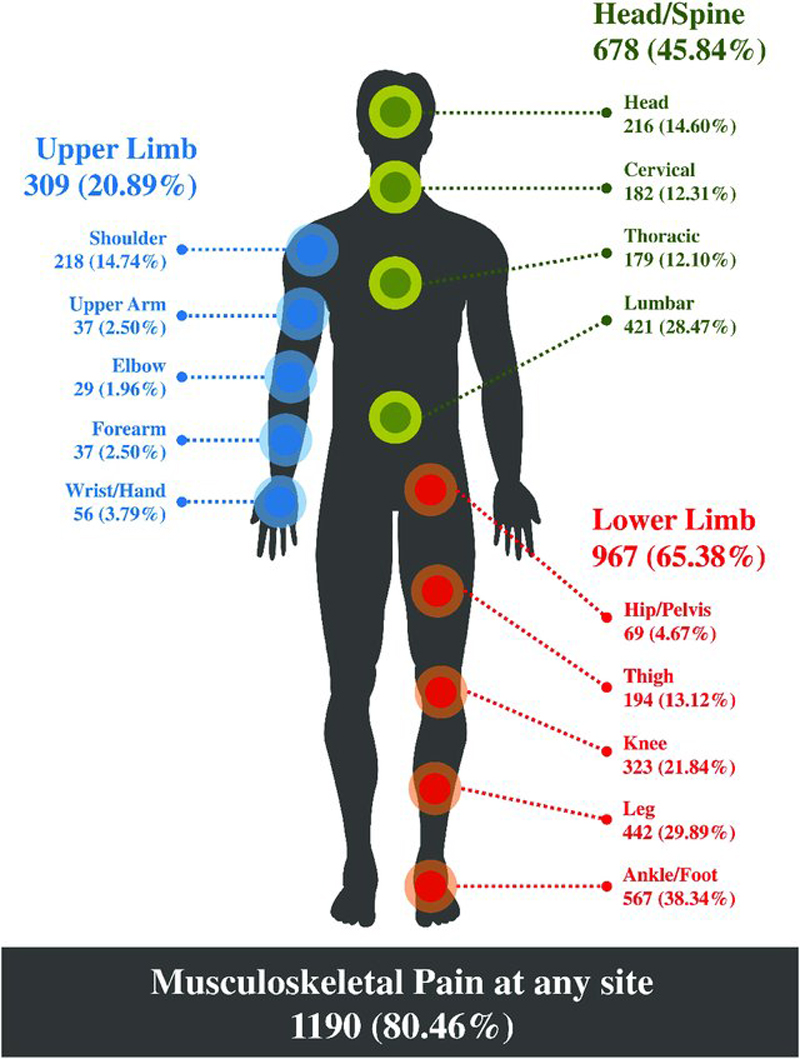
METHODS: Qualitative data were gathered to evaluate the outcomes of acupuncture and chiropractic (A/C) services for chronic musculoskeletal pain (CMP) using structured interview guides among patients with CMP (n = 90) and primary care providers (PCPs) (n = 25) purposively sampled from a managed care health care system as well as from contracted community A/C providers (n = 14). Focus groups and interviews were conducted patients with CMP with varying histories of A/C use. Plan PCPs and contracted A/C providers took part in individual interviews. All participants were asked about their experiences managing chronic pain and experience with and/or attitudes about A/C treatment. Audio recordings were transcribed and thematically coded. A summarized version of the focus group/interview guides is included in the Additional file 1.
RESULTS: We identified four themes around opioid use:
(1) attitudes toward use of opioids to manage chronic pain;
(2) the limited alternative options for chronic pain management;
(3) the potential of acupuncture and chiropractic (A/C) care as a tool to help manage pain; and
(4) the complex system around chronic pain management.
Despite widespread dissatisfaction with opioid medications for pain management, many practical barriers challenged access to other options. Most of the participants’ perceived A/C care as helpful for short term pain relief. We identified that problems with timing, expectations, and plan coverage limited A/C care potential for pain relief treatment.
There are more articles like this @ our:
CONCLUSIONS: These results suggest that education about realistic expectations for chronic pain management and therapy options, as well as making acupuncture and chiropractic (A/C) care more easily accessible, might lead to more satisfaction for patients and providers, and provide important input to policy makers.
TRIAL REGISTRATION: ClinicalTrials.gov NCT01345409
KEYWORDS: Acupuncture; Chiropractic; Chronic pain; Complementary medicine; Opioids; Primary care
From the FULL TEXT Article:
Background
Chronic pain conditions are pervasive public health issues that exact a staggering human and economic toll. Indeed, persistent pain affects an estimated 19% of adults in the U.S. [1] and results in $560 billion in direct medical treatment costs and lost productivity. This is especially troubling as these conditions disproportionately affect vulnerable populations. [2] The past decades have seen a dramatic escalation in the use of prescription opioids for the treatment of chronic non-cancer pain. [3] The period spanning the 1980’s through the early 2000’s has been widely described as an opioid epidemic [4] driven by the rising number of chronic non-cancer pain sufferers, liberalization of laws governing the use of opioids in pain treatment, aggressive pharmaceutical marketing, an acceptance of opioids as standard treatment of chronic pain, and mounting pressure on physicians to avoid undertreating pain. [3, 5–7]
Along with the rise in opioid prescribing for pain treatment [8] has come an increasing awareness of adverse outcomes, including addiction, transitioning to illegal drugs, and death (e.g., [9–14]) as well as concern about the limitations and efficacy of treatment with opioids in chronic pain management. [7, 15–17] In response, recent guidelines have been proposed for mitigating the risk of adverse outcomes [18], but evidence of effectiveness of many such guidelines is lacking. [19] Further, the clinical milieu has fostered a shift toward treatment that focuses on increasing patients’ functioning rather than on pain reduction. [20]
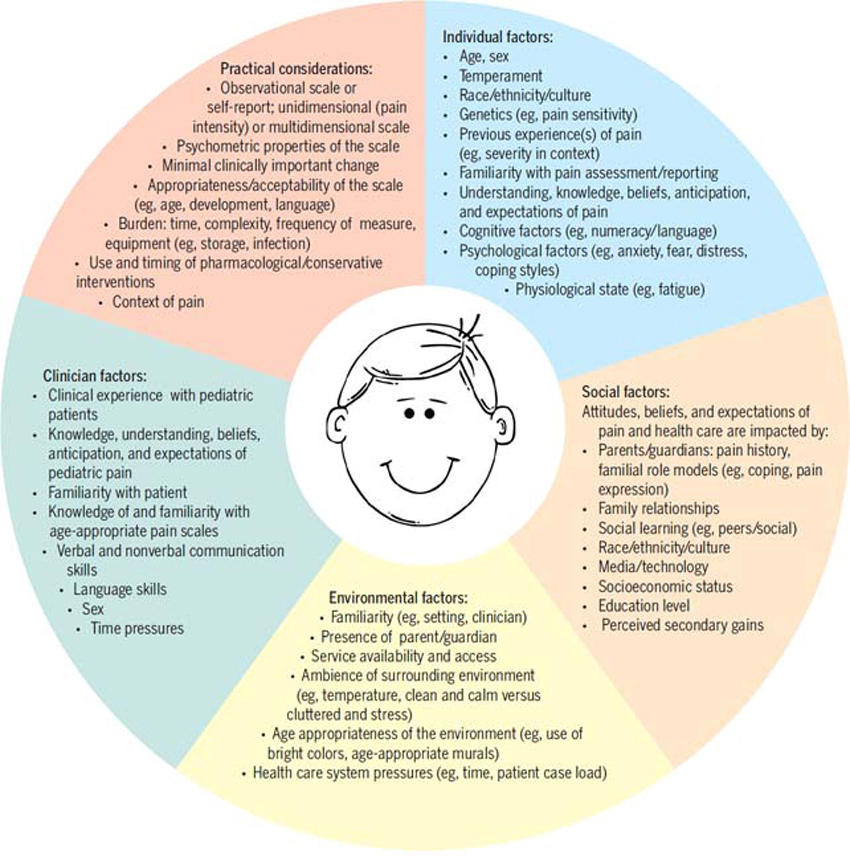
Redirecting patients with chronic pain from opioid therapy toward behavioral and other non-pharmacologic modalities has proven challenging. This is partly due to the paucity of comprehensive chronic pain management programs. [21] Additionally, only a few high-quality studies have assessed the effectiveness of interventions to taper off prescribed opioid use. [22, 23] While primary care providers (PCPs) are often aware of the risks and limitations of prescribing opioids as a monotherapy for pain, primary care practices often lack readily available systematic, integrated, and interdisciplinary treatment options [24, 25] or support for making prescribing decisions. [26] Both physicians and their patients are frustrated when alternatives to opioid therapy or tapering off opioid therapy are needed but effective and accessible alternatives are lacking.
Although other non-pharmacotherapy options exist [2, 27, 28], complementary and alternative medicine (CAM) may offer important non-opioid options for patients with chronic pain. In the United States, CAM treatment is used far more often for chronic musculoskeletal pain (CMP) than for any other condition. [29]
A recently published survey of patients with chronic pain at a large health maintenance organization, for example, reported that 58% of respondents had used acupuncture, chiropractic care, or both. [30] Among CAM treatments for CMP, acupuncture and chiropractic (A/C) care are the most highly accepted by physician groups [21, 32] even though such treatments are only modestly efficacious. [33–36] Nevertheless, the potential for adverse outcomes is low [37] and the treatment could facilitate self-care lifestyle changes considered instrumental to improve longer-term functioning for patients with CMP. [38, 39]
While much of the current literature has focused on the problems associated with opioid medications, a growing body of work is examining how to mitigate risks of adverse outcomes and increase the potential effectiveness of other pain therapies. Despite this literature, little has been written about the practical issues providers and patients face when trying to access alternatives to opioids for managing chronic pain and how both patients and their various providers view these issues. This paper fills this substantial gap in the literature by describing and comparing patient, PCP, and A/C providers’ perspectives of the treatment of chronic pain as a complex system in the context of their experiences accessing alternatives to opioids.
The goal of our analysis was to inform current debates about chronic opioid use for pain management and to describe the barriers providers face in changing therapeutic practice and CMP patients face in using such practices and co-managing their needs.
Read the rest of this Full Text article now!



Leave A Comment