Chronic Neck Pain Patients With Traumatic or Non-traumatic Onset: Differences in Characteristics.
A Cross-sectional Study
SOURCE: Scand J Pain. 2017 (Jan); 14: 1-8
Inge Ris, Birgit Juul-Kristensen, Eleanor Boyle,
Alice Kongsted, Claus Manniche, Karen Søgaard
Research Unit for Musculoskeletal Function and Physiotherapy,
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmark,
Campusvej 55, 5230 Odense M, Denmark;
BACKGROUND AND AIMS: Patients with chronic neck pain can present with disability, low quality of life, psychological factors and clinical symptoms. It is unclear whether patients with a traumatic onset differ from those with a non-traumatic onset, by having more complex and severe symptoms. The purpose of this study was to investigate the clinical presentation of chronic neck pain patients with and without traumatic onset by examining cervical mobility, sensorimotor function, cervical muscle performance and pressure pain threshold in addition to the following self-reported characteristics: quality of life, neck pain and function, kinesiophobia, depression, and pain bothersomeness.
METHODS: This cross-sectional study included 200 participants with chronic neck pain: 120 with traumatic onset and 80 with non-traumatic onset. Participants were recruited from physiotherapy clinics in primary and secondary health care. For participants to be included, they were required to be at least 18 years of age, have had neck pain for at least 6 months, and experienced neck-related activity limitation as determined by a score of at least 10 on the Neck Disability Index. We conducted the following clinical tests of cervical range of motion, gaze stability, eye movement, cranio-cervical flexion, cervical extensors, and pressure pain threshold. The participants completed the following questionnaires: physical and mental component summary of the Short Form Health Survey, EuroQol-5D, Neck Disability Index, Patient-Specific Functional Scale, Pain Bothersomeness, Beck Depression Inventory-II, and TAMPA scale of kinesiophobia. The level of significance for all analyses was defined as p<0.01. Differences between groups for the continuous data were determined using either a Student’s t-test or Mann Whitney U test.
RESULTS: In both groups, the majority of the participants were female (approximately 75%). Age, educational level, working situation and sleeping patterns were similar in both groups. The traumatic group had symptoms for a shorter duration (88 vs. 138 months p=0.001). Participants in the traumatic group showed worse results on all measures compared with those in the non-traumatic group, significantly on neck muscle function (cervical extension mobility p=0.005, cranio-cervical flexion test p=0.007, cervical extensor test p=0.006) and cervical pressure pain threshold bilateral (p=0.002/0.004), as well on self-reported function (Neck Disability Index p=0.001 and Patient-Specific Functional Scale p=0.007), mental quality of life (mental component summary of the Short Form Health Survey p=0.004 and EuroQol-5D p=0.001) and depression (Beck Depression Inventory-II p=0.001).
There are more articles like this @ our:
CONCLUSIONS: This study showed significant differences between chronic neck pain patients when differentiated into groups based on their onset of pain. However, no specific clinical test or self-reported characteristic could differentiate between the groups at an individual patient level.
IMPLICATIONS: Pressure pain threshold tests, cervical muscle performance tests and patient-reported characteristics about self-perceived function and psychological factors may assist in profiling chronic neck pain patients. The need for more intensive management of those with a traumatic onset compared with those with a non-traumatic onset should be examined further.
KEYWORDS: Chronic neck pain; Clinical outcomes; Cross-sectional; Patient reported outcomes; Whiplash associated disorder
From the Full-Text Article:
Introduction
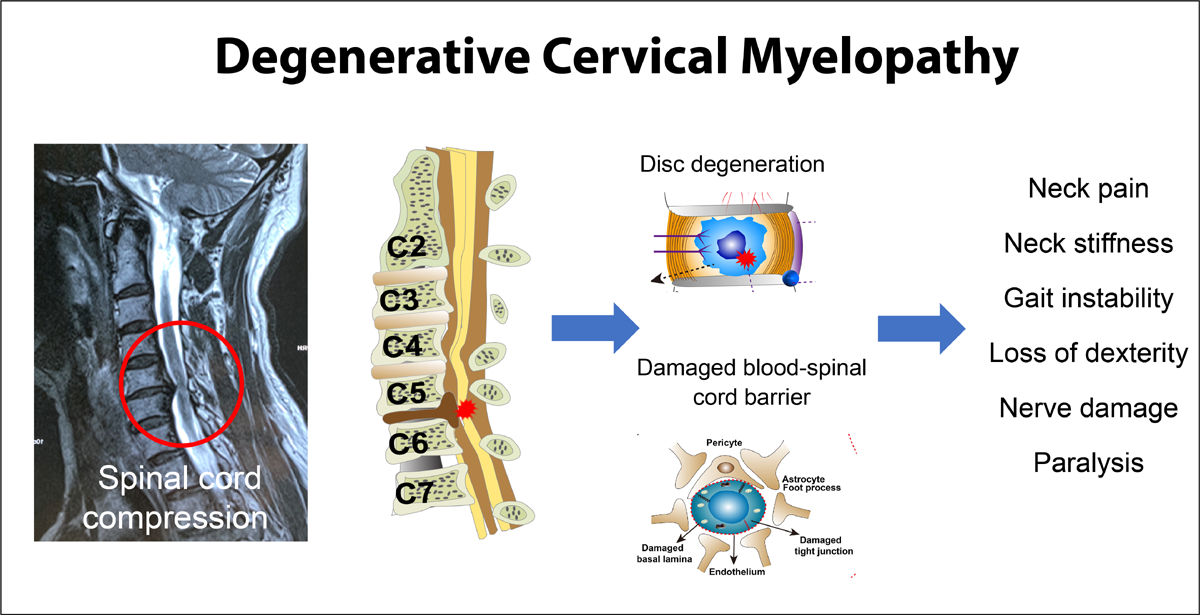
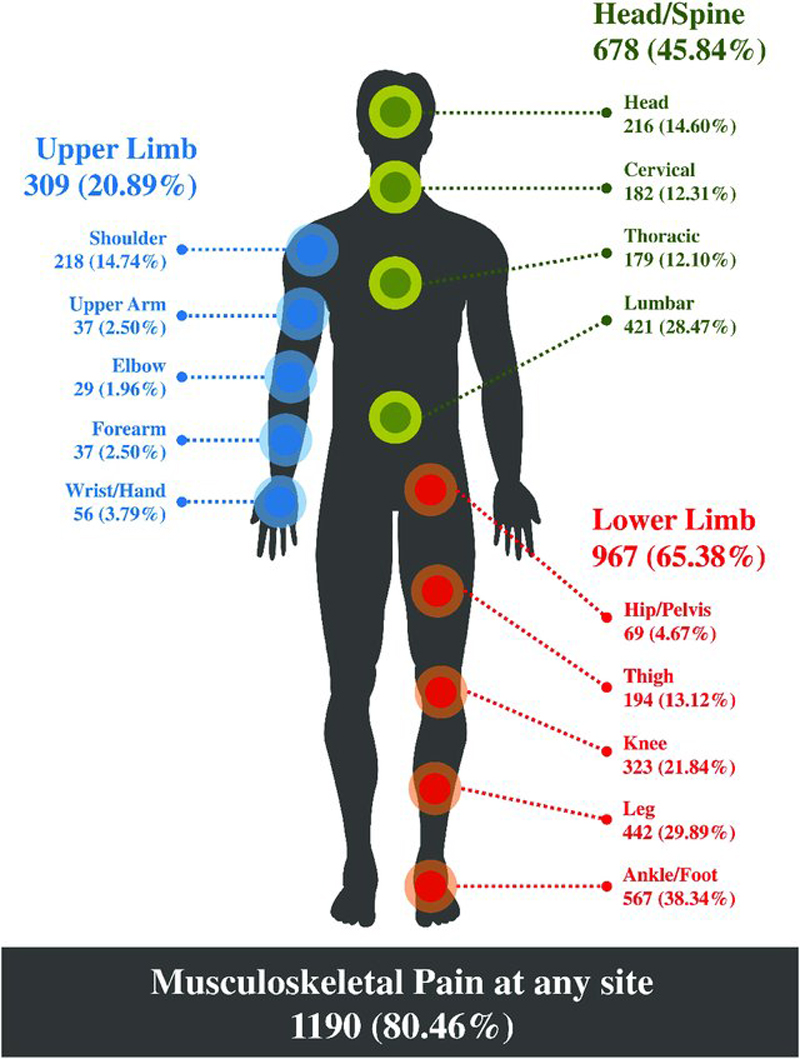
Most adults experience neck pain during their lifetime. The 12–month prevalence of neck pain is 30–50%, with activity-limiting neck pain varying between 1.7% and 11.5%. [1] In Denmark, 21% of patients referred to physiotherapy in primary care have neck pain. [2, 3] The cause of chronic neck pain can be traumatic (e.g. froma whiplash injury) or non-traumatic (e.g. work-related or degenerative). Regardless of the onset, chronic neck pain patients can present with a variety of symptoms including physical impairment, psychological distress, and social dysfunction. [4–6]
A traumatic onset of neck pain may relate to a whiplash injury. Approximately 50% will have on-going symptoms after a whiplash injury for months or years after the injury [8], and 10–20% will have severe pain after 7 years. [8, 9] These symptoms involve both physical and psychological changes. [10–14] Some of these symptoms may be due to central sensitisation mechanisms, a phenomenon seen mainly in traumatic neck patients. [12, 15] Non-traumatic chronic neck pain patients can also present with varying symptoms in addition to pain such as functional limitations [16] andp sychological changes. [17–19]
Some former studies have shown that the presentation of several symptoms may be dependent upon the onset being traumatic or non-traumatic: sensory alterations [15, 20], sensorimotor function [21], morphological changes [22], and specific psychological factors [23–25]; other studies have not found such group differences. [26–28]
Furthermore, whiplash is a controversial diagnosis. [29–32] As a consequence, in a recent report from Canada, the term ‘Whiplash’ in Whiplash Associated Disorders (WAD) was replaced with ‘Neck’ (Neck and Associated Disorders-NAD). [33] In other articles, WAD has been described as a medico-legal illusion [34] and a “man-made illness”. [35] In clinical practice and public debate, chronic neck pain patients with a traumatic onset or WAD are often considered more challenging regarding treatment than those with a non-traumatic onset. [36–40]
Read the rest of this Full Text article now!




Leave A Comment