Primary Spine Care Practitioners
SOURCE: Chiropractic & Manual Therapies 2011 (Jul 22); 19: 17 ~ FULL TEXT
The following is an interesting and well crafted article that posits yet another fanciful way to bring chiropractic “out of the closet”. I do have some issues with a few of Dr. Murphy’s recommendations, however:
1. In the Necessary Skill Set section of the article under point#2, he states that the “primary spine care practitioner” would employ those methods shown to be evidence-based, minimally invasive and cost-effective…one of them being the prescription of non-steroidal anti-inflammatory and non-opioid analgesics to their patients.
Our Iatrogenic Injury Page contains numerous articles detailing how NSAIDs and other analgesics are associated with the death of tens of thousands of people every year, for solely relying on them for pain relief. I just don’t see me EVER recommending them.
This is a genuine scientific conundrum:
how can anything that kills that many people still be referred to as “evidence-based”?UPDATE: (2-14-17) The Annals of Internal Medicine pre-published a new article titled:
and in it the authors stated:
The American College of Physicians (ACP) released updated guidelines this week that recommend the use of noninvasive, non-drug treatments for low back pain before resorting to drug therapies, which were found to have limited benefits. One of the non-drug options cited by ACP is spinal manipulation.
2. In the Obstacles To The Implementation section under point#5, Dr. Murphy states that “For whatever profession or professions that respond to the need for a primary spine care practitioner, this will be a significant disruption to the traditional practice patterns or self-image of these professions. As a result, the role that we are introducing here will be actively resisted”. Oh how true!
When you look closely at the “expanded practice” movement, the first thing I noticed was that this movement is being promoted by the chiropractic schools that have the lowest enrollment of students.
I suspect that they are hoping to (or already have) developed an “expanded practice” program that will attract more students, and that’s understandable, if expanding your income is your primary objective.
3. Finally, there is the subtle hint that becoming an “expanded practice chiropractor” (or “medi-practor”) will increase the doctor’s “market share”. That may even be true. But, if that also means embracing the kind of evidence-based care that kills thousands every year, I say “No thank you, sir”.
Please don’t get me wrong: I have tremendous respect for Dr. Murphy and the other authors of the following article.
This article is very well written and logical… up to a point. I am posting it on our blog because I agree that our profession needs to review this material and see if and how it can be tweaked. Most of their suggestions are valid. I just don’t see the need to grab for prescription rights….not when there’s such considerable scientific evidence for recommending Omega-3 fatty acids for pain relief.
I hope you will enjoy the following new article:
The Establishment of a Primary Spine Care Practitioner and its Benefits to Health Care Reform in the United States
Donald R Murphy
Brian D Justice
Ian C Paskowski
Stephen M Perle
Michael J Schneider
INTRODUCTION
One of the most talked about issues in the United States (US) is health care reform. In other countries as well, discussion commonly revolves around the issue of how health care services can be improved while containing costs. Many in the US have described the current health care situation as a “crisis” [1-4]. In March 2010, the US Congress passed and the President signed into law the Affordable Care Act, which puts in place comprehensive health care reform measures [5]. While various models for providing care to patients have been considered, such as accountable care organizations [6], it is recognized that any meaningful approach to health care reform will require three goals to be achieved:
1. improved patient health;
2. improved patient experience;
3. decreased per capita costs [7].
Spine-related disorders (SRDs) are among the most common, costly and disabling problems in Western society. For the purpose of this commentary, we define SRDs as the group of conditions that include back pain, neck pain, many types of headache, radiculopathy, and other symptoms directly related to the spine. Virtually 100% of the population is affected by this group of disorders at some time in life. Low back pain (LBP) in the adult population is estimated to have a point prevalence of 28%-37%, a 1-year prevalence of 76% and a lifetime prevalence of 85% [8, 9]. Up to 85% of these individuals seek care from some type of health professional [10, 11]. Two-thirds of adults will experience neck pain some time in their lives, with 22% having neck pain at any given point in time [12].
Read the rest of this Full Text article now!


I’ll need to read more of this but for now I just say that I align myself with the expand care movement. However, I view expanded care in three ways that stem from scope of practice ideas. One is where scope of practice is defined by the modalities used but not by conditions treated. The other is by conditions treated and not by modalities used. The last is a combination of the previous two.
One thing I can say for sure is that I do NOT want chiropractic to be pigeon-holed as spine specialists only.
The other thing I can say for sure is that I do not want chiropractic to be only “non-invasive.”
This of course leaves many ways in which a final scope notion could emerge depending on the degree to which one goes on any of these parameters. Never the less, the overarching view should be constructed in ways so that when better treatments come along then we will be able to use them. Keep in mind that exercise, SMT, acupuncture and massage have only been shown to be mild to at best moderately effective. Expect progress and change.
As a final note, I’m starting to move in a direction where we get rid of the term “chiropractic subluxation” but haven’t fully gone that way yet.
Hi Dr Szlazak,
It saddens me to see that some DCs would prefer that the debate over the use of terms like “adjust” and “subluxation” would go away. I guess I am a traditionalist. Of course, I learned philosophy from Virgil Strang, so I am biased.
I have no objection to DC expanding their practice, and I don’t believe the profession is threatened by that wish…however, it IS threatened by organized medicine, who is clearly in an uproar against poaching on their preserve.
Here are two reasons I think the term chiropractic subluxation could be replaced. They are mostly from a pragmatic or utility point of view and are based on some assumptions which of course maybe incorrect.
Who really is the target audience for the terms “chiropractic subluxation?”
If it’s patients/public then I don’t think replacing or even using those terms matters all that much.
If it’s chiropractors then I think these terms have evolved away from initial ideas and more specific categories could be used now to describe various spinal disorders that respond to SMT. Basically, I view “chiropractic subluxation” as an older category that _could be_ broken up into newer categories with more specific or accurate definitions.
While I don’t necessarily want to be pigeon holed either, the spine care pie is so large that if pie were given to us I would be okay with it.
Despite chiropractic’s longevity, the profession has not succeeded in establishing cultural authority and respect within mainstream society, and its market share continues to dwindle. I am concerned that the common perception (which is well supported, in my experience) that chiropractors are only interested in “selling” a lifetime of chiropractic visits may be one of the primary factors behind our low standing in the minds of members of the public [1]. The recommendation for repetitive life-long chiropractic treatment compromises any attempt at establishing a positive public health image and needs to change. Public health is ultimately about self-empowerment and teaching people how to take care of themselves, with an emphasis on prevention and health maintenance. The chiropractic profession should adopt the American Public Health Association’s (APHA) scientifically-grounded emphasis on nutrition and exercise as the “keys to wellness”
I see the future chiropractor as a “non-surgical spine & musculoskeletal specialist”, enjoying full cultural authority, legitimacy and trustworthiness – but only under the following circumstances:
1) Chiropractic must abandon the Subluxation as a foundational premise.
The maxim in the computer world is: Garbage in, garbage out. Consequently, if we present a false premise, any conclusions based on this premise must also be false, to wit, the subluxation! The chiropractic subluxation stands pretty much today as it did at the dawn of the 20th century: an interesting notion without validation.
The chiropractic profession has an obligation to actively divorce itself from metaphysical explanations of health and disease as well as to actively regulate itself in refusing to tolerate fraud, abuse and quackery, which are much more rampant in our profession than in other healthcare professions [2.] This must be done on an individual practitioner basis as well as by the political, educational and regulatory bodies. In this way the profession can fulfill its responsibility to the social contract. This will dramatically increase the level of trust in, and respect for, the profession from society at large.
We must finally come to the painful realization that the chiropractic concept of spinal subluxation as the cause of “dis-ease” within the human body is an untested hypothesis [3]. It is an albatross around our collective necks that impedes progress. There can be no unity between the majority of non-surgical spine specialist chiropractic physicians and the minority of chiropractors who espouse metaphysical, pseudo-religious views of spinal subluxations as “silent killers” [4]. The latter minority group needs to be marginalized from the mainstream majority group, and no longer should unrealistic efforts be made toward unification of these disparate factions within the profession.
The chiropractic profession must establish a clear identity and present this to society. In the beginning, DD Palmer invented a lesion, and a theory behind this lesion, and developed a profession of individuals who would become champions of that lesion. This is not what credible professions do. A credible profession is one that is established by society to meet a need that society itself has decided must be met [5]. Based on all the evidence regarding chiropractic practice and education, there is only one societal need (but it is a huge one) that chiropractic medicine has the potential to meet: non-surgical spine care. Our education and training is focused on the spine, and clearly if there is a common bond among all chiropractors, it is spine care [6.] While there are a variety of practitioners who offer spine care (physical therapists, osteopaths, movement specialists, and massage therapists) there is no physician-level specialty that has carved a niche as society’s one-and-only non-surgical spine specialist whose expertise is focused on the diagnosis and management of spine disorders.
2) Chiropractic education must be science-based, must be standardized, and must fall under the auspices of state universities.
One of the problems that are encountered frequently in our chiropractic educational institutions is the perpetuation of dogma and unfounded claims. Examples include the concept of spinal subluxation as the cause of a variety of internal diseases and the metaphysical, pseudo-religious idea of “innate intelligence” flowing through spinal nerves, with spinal subluxations impeding this flow[18]. These concepts are blatantly lacking in a scientific foundation [3][7][8]and should not be permitted to be taught at our chiropractic institutions as part of the standard curriculum. Much of what is passed off as “chiropractic philosophy” is simply dogma [9], or untested (and, in some cases, untestable) theories [3] which have no place in an institution of higher learning, except perhaps in an historical context. Faculty members who hold to and teach these belief systems should be replaced by instructors who are knowledgeable in the evidence-based approach to spine care and have adequate critical thinking skills that they can pass on to students directly, as well as through teaching by example in the clinic.
Ideally, the profession must undergo its own version of the Flexner Report that medicine underwent, and/or the Selden Commission Report and Educational Enhancement Project that podiatric medicine subjected itself to. That is, we must take a critical look at our educational institutions, find what is substandard, correct those deficiencies and standardize education across the board. Additionally (and this is essential), chiropractic education (manual medicine, if you will) must eventually merge with state university medical schools.
The long term vision must be to integrate fully with mainstream medicine through the elimination of private, self-serving, tuition-based chiropractic colleges (I mean so-called, “Universities” –“whatever you want we’ll make up the course and offer it to you, as long as you pay, pay, pay the tuition…and once you do that we’ll make up a “Certification” course, where you’ll pay some more, and then a “Diplomate” course, where you’ll pay even more, and then you’ll have to keep these certifications up to date with yearly courses and conferences…. blah, blah, blah…..!), and the establishment of chiropractic manual medicine departments under the support of the state university system, which, in and of itself, the university will attract a higher caliber chiropractic student, who will already have an entrance B.S. degree, and who will undertake the basic sciences together with his/her medical counterpart, which will consist of 4 years of standardized science-based education. Understandably, there will be unavoidable intellectual collaboration, discussion and the understanding of the roles of each health care provider in the public domain.
The second phase of the student’s education will commence at the termination of the basic science educational stage, whereupon the medical student will follow his/her studies in allopathic medicine, and the chiropractic student will pursue his/her chiropractic studies of an EVIDENCE-BASED, STANDARDIZED curricula for the following 4 years. Upon matriculation, both medical and chiropractic graduates will undertake and complete appropriate internship and residency programs. Graduated Chiropractic Physicians will follow a 3-year residency: Internal Medicine (1 year) and Orthopedics/Physical Medicine & Rehabilitation (2 years).
It is essential that the chiropractic profession establish hospital-based residencies [10]. There is a significant void in how chiropractic graduates develop any meaningful hands-on clinical experience with real patients in real life situations. It is widely recognized in medical and podiatric education that abundant exposure to clinical environments is essential to developing top-quality professions. The Council on Chiropractic Education requirement of 250 adjustments forces interns to use manipulation on patients whether they need it or not, and the radiographic requirement forces interns to take radiographs on patients whether they need them or not. Rather than focus on interns meeting certain numerical requirements, interns should be encouraged to develop clinical decision making and patient management skills. Further, the emphasis on achieving a certain number of procedures as opposed to the acquisition of skill and knowledge impedes the development of professional moral reasoning by training interns to use patients as a means to meet their own goals, rather than focusing on the needs of the patients themselves. The chiropractic internship should, as with medicine and podiatry, occur after graduation. Chiropractic regulatory bodies such as state boards of chiropractic medicine should move in the direction of requiring the completion of postgraduate residency training as a condition of licensure.
What this will mean for chiropractic is a giant step towards Cultural Authority and Legitimacy. It will mean a higher standard of chiropractic student (intellectually, morally & ethically) entering the State University of their choice, i.e., a real university offering transferable subject matter to any other university in the nation). It will also mean an enhanced understanding and respect between the two healthcare professions, which will then result in later professional corroboration and professional inter-referral mind-set based on mutual trust, respect and the appreciation of the individual skill-sets each practitioner brings to the table.
3) Chiropractic must seriously consider amalgamating with the physical therapy profession by means of education and attaining the Doctor of Manual Medicine (DMM) degree
Because the chiropractic profession has a very unique skill set that is desperately and immediately needed within the health care system – non-surgical spine (MSK) care – the PTs and DCs could unite forces and collectively stake a claim to all MSK care, and partition primary care into two basic categories:
(1) primary care for internal disorders which will be triaged and managed by PCPs, PAs, NPs, and DOs, and
(2) primary care for musculoskeletal disorders, which will be triaged and managed by DCs and PTs…along with some PM&R docs and DOs who have an MSK focus.
My sense is that this may be the opportunity we are missing!
It seems reasonable and pragmatic that chiropractic could change its name to “Doctor of Manual Medicine” (DMM) – remember the chiropodists with no cultural authority, who are now podiatrists with all kinds of cultural authority? – and integrate itself into a state university Doctor of Physical Therapy (DPT) program. Doctors of Physical Therapy have long enjoyed cultural authority, legitimacy and trustworthiness and, perhaps with a post-graduation residency in orthopedics (3 years), a Doctor of Manual Medicine (DMM) could be conferred? Such a paradigm shift would immediately position [chiropractic] within mainstream health care, thus affording the gratification of the cultural authority, legitimacy and trustworthiness so dearly sought after, as well as the willing and free-flow of referrals of those patients suffering uncomplicated spine & musculoskeletal injuries and/or conditions, from medical physicians, and others, to the DMM. This is, of course, dependent upon #1 above.
No matter how one looks at it, or what one would like reality to be, chiropractic medicine is about back pain, neck pain and headache. Instead of fighting that fact (or denying it), we should embrace it fully and focus on becoming society’s “go-to” profession for disorders in this area.
First, spine-related pain is one of the largest markets in all of health care. Considering neck/arm pain, back/leg pain and headache, virtually 100% of the population is potentially included [11][12] (contrast this with the fact that only 5% of the population currently see a chiropractor [3]).
Second, no medical specialty has successfully carved a niche for itself in this area (although the physical therapy profession is moving rapidly in this direction).
Third, spine-related disorders create a great deal of suffering on the part of patients, in addition to exacting great costs on employers, the healthcare system and society at large. Providing much-needed high quality care to individuals suffering from spinal pain, as well as initiating and taking part in public health campaigns designed to educate people about spinal pain, would be a great service to society, and would bring millions of new patients to the offices of Doctors of Manual Medicine [chiropractic], patients who would not ordinarily consider seeing a chiropractic physician.
The chiropractic profession fairly recently had a unique opportunity to catapult itself into the role of society’s non-surgical spine specialists. In 1994 the Agency for Health Care Policy and Research (AHCPR) released its guidelines on the management of acute low back pain in adults [13]. These guidelines recommended spinal manipulation as one of the only treatments for which adequate evidence existed for its efficacy. The report received a great deal of media coverage, with some media outlets actually mistakenly identifying “chiropractic”, rather than “manipulation” as the recommended first-line approach. Leadership with any vision at all could have used this as a springboard to moving chiropractic into the mainstream as the premier non-surgical spine specialists in society. However, the profession did not jump at the chance, largely, in my view, for fear of being “limited” by the image. Ironically, the profession chose to avoid being “limited” to the management of a group of disorders (back pain, neck pain and headache) that affect virtually 100% of the population through all stages of life [14]. In the interim it has seen its market share dwindle from 10% of the population [4] to less than 5% [3][15]. Even amongst patients with back pain, the proportion of patients seeing chiropractors dropped significantly between 1987 and 1997, a period of time in which the proportion seeing both medical doctors and physical therapists increased [16].
The convoluted thinking of chiropractors constantly amazes me, inasmuch as it is interesting that chiropractors have traditionally prided themselves on being “holistic”. The emerging model of modern spine care is the “biopsychosocial” model [17]. That is, it is increasingly recognized that in order to provide optimum care for patients with spine-related disorders, one has to consider the whole person. Thus, non-surgical spine care provides chiropractic medicine with a wonderful opportunity to provide truly holistic care for patients, and to be recognized for expertise in this area. This would certainly be a drastic departure from the reductionistic, subluxation-only approach, which “reduces” the cause and care of health problems to a spinal subluxation. Further, because the biopsychosocial approach often requires multidisciplinary involvement, embracing this model will further help to integrate chiropractic medicine into mainstream health care.
Certainly there is opportunity for chiropractic medicine to become what it can and should be: a profession of non-surgical spine specialists who not only offer one useful modality of treatment for spinal pain (manipulation), but offer something much greater and more important – expertise in the diagnosis and management of spinal pain patients. This includes understanding the vast mechanisms of spinal pain as well as diagnosis, treatment and coordination of the treatment with other members of the healthcare team. It also means mastering a variety of non-surgical methods other than just manipulation that are useful in the management of patients with spinal pain. But, most importantly, it means becoming experts in patient management, i.e., helping patients overcome spinal pain, whether that means providing adjustments, exercise, referral for short-term medication use and/or education regarding the issues related to LBP provided in a cognitive-behavioral context. Currently, there is no profession that adequately fills that role, although as noted earlier, the physical therapy profession is moving quickly in this direction.
The opportunity is there for us to correct our mistakes, but we must act now. The only question is whether the chiropractic profession has the integrity, vision and self-reflection required to make the necessary changes. Time will tell…..but don’t hold your breath!
References
1. Gallup poll: Americans have low opinion of chiropractors’ honesty and ethics
Dynam Chiropr 2007., 22(3):
2. Foreman SM Stahl MJ: Chiropractors disciplined by state chiropractic board and a comparison with disciplined medical physicians.
J Manipulative Physiol Ther 2004, 27(7):472-476
3. Keating JC Jr., Charlton KH, Grod JP, Perle SM, Sikorski D, Winterstein JF: Subluxation: dogma or science?
Chiropractic & osteopathy 2005, 13:17
4. Carter R: Subluxation – the silent killer.
5. Hughes EC: Professions. Daedalus 1962, 92:655-668.
6. Nelson CF Lawrence DJ, Triano JJ, Bronfort G, Perle SM, Metz RD, Hegetschweiler K, LaBrot T: Chiropractic as spine care: a model for the profession. Chiropr Osteopat 2005, 13:9.
7. Mirtz TA: The question of theology for chiropractic: A theological study of chiropractic’s prime tenets. J Chiropr Human 2001., 10(1):
8. Mirtz TA: Universal intelligence: A theological entity in conflict with Lutheran theology. J Chiropr Human 1999., 9(1):
9. Seaman D: Philosophy and science versus dogmatism in the practice of chiropractic. J Chiro Human 1998, 8(1):55-66.
10. Wyatt LH Perle SM, Murphy DR, Hyde TE: The necessary future of chiropractic education: a North American perspective. Chiropractic & osteopathy 2005, 13(10):1-15.
11. Cote P Cassidy JD, Carroll LJ, Kristman V: The annual incidence and course of neck pain in the general population: a population-based cohort study.Pain 2004, 112(3):267-273.
12. Cassidy JD Cote P, Carroll LJ, Kristman V: Incidence and course of low back pain episodes in the general population. Spine 2005, 30(24):2817-2823
13. Bigos S, Bowyer O, Braen G Brown K, Deyo R, Haldeman S: Acute Low Back Problems in Adults Clinical Practice Guideline Number 14 AHCPR Pub No 95-0642 Rockville, MD Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services.
14. Hartvigsen J, Christensen K: Pain in the back and neck are with us until the end: a nationwide interview-based survey of Danish 100-year-olds. Spine 2008, 33(8):909-913.
15. Barnes PM Powell-Griner E, McFann K, Nahin RL.: Complementary and alternative medicine use among adults: United States, 2002. Adv Data 2004, 343:1-19.
16. Feurestein M, Marcus SC, Huang GD: National trends in nonoperative care for nonspecific back pain. Spine J 2004, 4(1):56–63.
17. Pollard H Hardy K, Curtin D: Biopsychosocial model of pain and its relevance to chiropractors. Chiropr J Aus 2006, 36(3):92-96.
18. Palmer College of Chiropractic – Identity (2013)
Hi Peter
I read your post with interest.
I have heard the argument that the word “subluxation” is leading us to ruin, and I just don’t buy it.
Here’s the definition of subluxation, as adopted by the American Chiropractic Association and the Association of Chiropractic Colleges
“A subluxation is a complex of functional and/or structural and/or pathological articular changes that compromise neural integrity, and may influence organ system function and general health.”
[1]
There is simply nothing to argue about. Joint fixation leads to abnormal changes, and the neurologic consequences are unpleasant. Finally, most patients agree that Chiropractic Care is corrective of their complaints.
Further, recommending Maintenance or Wellness Care is NOT a bad idea, as you maintain. There is a growing body of research that suggests that continued (non-symptomatic) care IS beneficial. [2]
Finally…every Profession has a small number of questionable individuals, who *might* reflect on the rest. However, no one has given up on Medicine because there are a few bad apples in their pie, so why would it happen to us???
What set us back (IN REALITY) was decades of organized mis-information campaigns, sponsored first by the AMA, and later by a tiny group of pseudo evidence-based malcontents. [3, 4] If enough people hear those lies and rumors, for DECADES, of course it will have an adverse impact on our *assimilation*.
Your suggestion that Chiropractic Education be assimilated by the University system has missed the boat. It’s already been tried, and has failed miserably. At least three different Universities, which adopted DC programs failed in the last 15 (or so) years. I’d LOVE to see DC students (and our Schools) get the same breaks other Universities get, but I’m not holding my breath.
REFERENCES:
1. What is The Chiropractic Subluxation?
http://www.chiro.org/LINKS/subluxation.shtml
2. Maintenance Care, Wellness and Chiropractic
http://www.chiro.org/research/ABSTRACTS/Maintenance_Care.shtml
3. Chiropractic Antitrust Suit ~ Wilk, et al vs. the AMA, et al
http://www.chiro.org/Wilk/
4. The Quack Watchers
http://www.chiro.org/LINKS/QUACKWATCHERS.shtml
Hello Frank:
I appreciate your position and comments. Thank you.
With all due respect there is plenty to argue about…….!
Whereas the definition promulgated by the ACA and ACC is an interesting one, it is certainly an eon-removed from the original DD Palmer definition – you know, the one that all of the scientific world identifies us with!
Although the ACC model of subluxation has been widely endorsed and has become somewhat of a “standard” for the chiropractic profession, I do have a problem with it.
First, the hypothesis that subluxation is some “complex of functional and/or structural and/or pathological articular changes that compromise neural integrity” is offered without qualification, that is, without mention of the uncertain, largely untested quality of this claim. The nature of the supposed compromise of “neural integrity” is unmentioned. Just saying it, doesn’t make it so.
Secondly, the dogmatism of the ACC’s unsubstantiated claim that subluxations “may influence organ system function and general health” is not spared by the qualifier “may.” The phrase could mean that subluxations influence “organ system function and general health” in some but not all cases, or that subluxation may not have any health consequences. Although the latter interpretation is tantamount to acknowledging the hypothetical status of subluxation’s presumed effects, this meaning seems unlikely in light of the ACC’s statement that chiropractic addresses the “preservation and restoration of health” through its focus on subluxation. Both interpretations beg the scientific questions: do subluxation and its correction “influence organ system function and general health”?
Lastly, the ACC claims that chiropractors use the “best available rational and empirical evidence” to detect and correct subluxations. This strikes me as pseudoscience, since the ACC does not offer any evidence for the assertions they make, and since the sum of all the evidence that I am aware of does not permit a conclusion about the clinical meaningfulness of subluxation. To the best of my knowledge, the available literature does not point to any preferred method of subluxation detection and correction, nor to any clinically practical method of quantifying compromised “neural integrity,” nor to any health benefit likely to result from subluxation correction, regardless of whether “Joint fixation leads to abnormal changes, and the neurologic responses to it are unpleasant” (Classic “Post Hoc Ergo Proper Hoc” fallacy!).
I believe that whether chiropractors are actually treating lesions, or not, is a question of immense clinical and professional consequence. Resolution of the controversy will not be found through consensus panels nor through semantic tinkering, but through proposing and testing relevant hypotheses.
There is precious little experimental evidence available supporting the theoretical construct of the chiropractic subluxation. I believe it to be a legitimate, but untested hypothesis (in scientific terms). The evidence to date hardly supports the widespread notion among the chiropractic community that it is meaningful in human health and disease. It is this notion still prevalent today in chiropractic that brings ridicule from the scientific and mainstream health care communities. Over the years (last two decades, or so) many chiropractors preeminent theoretical constructs remains unsubstantiated and largely untested. There has been little if any substantive experimental evidence for any operational definition of the chiropractic lesion offered in clinical trials.
Notwithstanding strong intra-professional commitment to the subluxation construct and reimbursement strategies that are legally based upon subluxation, there is today no scientific “gold standard” for detecting these reputedly ubiquitous and supposedly significant clinical entities, and inadequate basic science data to illuminate the phenomenon . The chiropractic subluxation continues to have as much or more political than scientific meaning.
I don’t think the clinical meaningfulness, if any, of subluxation can be established by definition. The notion that subluxation is inherently pathological, perhaps because some dictionary equates subluxation with ligamentous sprain, does not mean that joint dysfunction merits clinical intervention
The magic and mystery of subluxation theories all too frequently direct the chiropractor’s attention to a search for the “right” vertebra, instead of addressing the legitimate question of whether subluxation (or any other rationale for manipulation) may be relevant in a patient’s health problem?
Many chiropractors bombard themselves and the public with subluxation rhetoric, but rarely hint at the investigational status of this cherished idea.
Hypothetical constructs involve tentative assertions about physical reality. They serve as essential tools in the development of science, and permit the empirical testing of the non-obvious. However, when the speculative nature of an hypothesis or hypothetical construct is not made obvious, an otherwise acceptable proposition becomes a dogmatic claim. Such is the history of subluxation in chiropractic.
The dogma of subluxation is perhaps the greatest single barrier to professional development for chiropractors. It skews the practice of the art in directions that bring ridicule from the scientific community and uncertainty among the public. Failure to challenge subluxation dogma perpetuates a marketing tradition that inevitably prompts charges of quackery. Subluxation dogma leads to legal and political strategies that may amount to a house of cards and warp the profession’s sense of self and of mission. Commitment to this dogma undermines the motivation for scientific investigation of subluxation as hypothesis, and so perpetuates the cycle.
It seems to me that as long as we as a profession rely on CONSENSUS STATEMENTS concerning subluxation dogma as though it were validated clinical theory, the cultural authority we so desperately need to enter mainstream health care, will continue to elude us.
With regard to Maintenance Care: My suggestion that “maintenance care” or “wellness care” is inappropriate is directed ONLY to those chiropractors (the majority, I fear), who sell life-long treatment programs to HEALTHY people, on the ASSUMPTION that chiropractic adjustments of magical “subluxations” keep HEALTHY people HEALTHY (remember there is no SCIENTIFIC PROOF that it is efficacious!) I am well aware of the handful of studies that support maintenance care – but if you read them carefully you’ll notice that they are designed for REAL patients under management for RECURRING BACK PROBLEMS, in an attempt to deter recidivism.
I wish I could agree with you regarding your statement that “every profession has a small number of questionable individuals, who *might* reflect on the rest”. Most polls put chiropractors far below the MD with regard to cultural authority, legitimacy and trustworthiness! Chiropractors, generally, are looked upon as the “Gizmo Guys”, and as charlatans, and in many cases a step above the second-hand car salesman! The fact that our market-share now hovers somewhere between 3%-5%, from a high of about 15% just a decade ago, should tell you something!
As to your assessment that chiropractic has “missed the boat”, through the failures over the past 15 years of being assimilated into REAL university settings, begs the question, WHY? Might it be because of our metaphysical, pseudoscientific, semi-religeous, magical thinking basis we rely on? I know of one instance where the effort of becoming a REAL PROFESSION was scuttled by our own “Fountain Head” – Palmer College! We are indeed our own worst enemy, are we not?! Now that we realize that in order to survive, we MUST be accepted into mainstream health care, we lean towards our usual old “Pity Party” antics by trying to bamboozle the states legislatures with semantical gobblydegook and filing law suits, rather than acting as adults and PROVING ourselves worthy on a fundamental SCIENTIFIC level. The main impediment in our acceptance as a “real” health care profession is the basic premise of the “magical” subluxation. Get rid of it, and the “profession” will be a big step closer to being considered legitimate rather than a bunch of bug-eyed, frothing-at-the-mouth, finger-pointing charlatans.
In summary, I stand by my assertions, that if we want to be included in mainstream health care, we must get rid of the subluxation theory, become part of state universities in terms of education, and develop chiropractic physicians who are evidence-based, ethical and upstanding. At this point in time the most expedient method would be to join ranks with the physical therapists,implement a Doctor of Manual Medicine degree (DMM),by taking their DPT degree course, do a 3-year residency (1 year internal medicine; 2-years orthopedics/rehabilitation) and graduate with the DMM degree. That would immediately bestow the mantle of cultural authority, legitimacy and trustworthiness upon us, and allow us to function as PRIMARY SPINE CARE PROVIDERS. We could work side-by-side with the physical therapy profession – there is certainly far more non-specific, spine-pain/musculoskeletally compromised patients available than our two professions could handle!
But, what do we do? We circle the wagons…. and you know the rest!
The chiropractic leadership MUST step-up and make the paradigm shift – or slowly watch the demise of chiroipractic as a profession……we have a long road to hoe!
Respectfully,
Peter G. Furno, D.C.
Indianapolis.
Dr Furno,
You make some excellent points but miss the big picture. The article in question discusses the role of chiropractors in primary care. This means screening patients, deciding the best plan of care, referring out, collaborating with other health professionals, giving general health advice to promote the WHO definiton of health, promoting public health, and caring for patients. Caring for patients means treating their problem and managing their problem which may be acute or chronic. Care includes chiropractic care, ergonomic advice, life-style advice. Further care may include prevention. This depends on the patients’ wishes. And further care may concentrate on performance: dancers, athletes or people that just want to live better (and longer!)
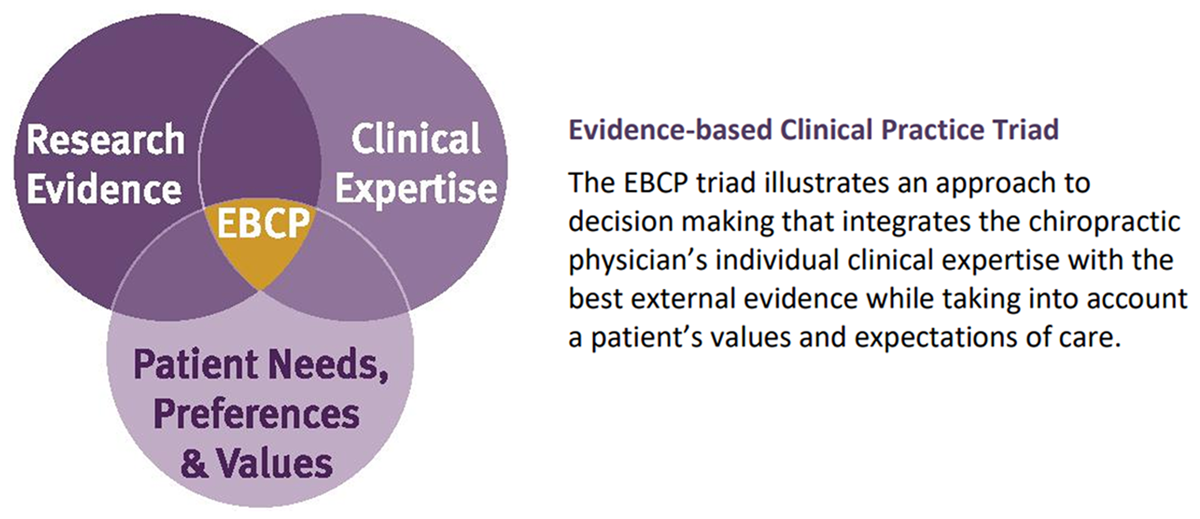
Evidence based care includes applying the best evidence, patient’s wishes, and the experience of the practitioner. Patient-centred care includes predictive, preventive and personalised care. Chiropractic primary care employs the knowledge, skills, values/personal attributes and competences of the practitioner for the benefit of the patient.
Have a wonderfuld day.
Kind regards, Baiju