Lower Back Trauma
We would all like to thank Dr. Richard C. Schafer, DC, PhD, FICC for his lifetime commitment to the profession. In the future we will continue to add materials from RC’s copyrighted books for your use.
This is Chapter 12 from RC’s best-selling book:
“Chiropractic Posttraumatic Rehabilitation”
These materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
CHAPTER 12: LOWER BACK TRAUMA
Although it is easier to teach anatomy by dividing the body into arbitrary parts, a misinterpretation can be created. For instance, we find clinically that the lumbar spine, sacrum, ilia, pubic bones, and hips work as a functional unit. Any disorder of one part immediately affects the function of the others.
BACKGROUND
A wide assortment of muscle, tendon, ligament, bone, nerve, and vascular injuries in this area is witnessed during posttrauma care. As with other areas of the body, the first step in the examination process is knowing the mechanism of injury if possible. Evaluation can be rapid and accurate with this knowledge.
Low-back disability rapidly demotivates productivity and athletic participation. The mechanism of injury is usually intrinsic rather than extrinsic. The cause can often be through overbending, a heavy steady lift, or a sudden release —all which primarily involve the muscles. IVD disorders are more often, but not exclusively, attributed to extrinsic blows and intrinsic wrenches. An accurate and complete history is invariably necessary to offer the best management and counsel.
INITIAL ASSESSMENT
A player injured on the field or a worker injured in the shop should never be moved until emergency assessment is completed. Once severe injury has been eliminated, transfer to a back board can be made and further evaluation conducted at an aid station.
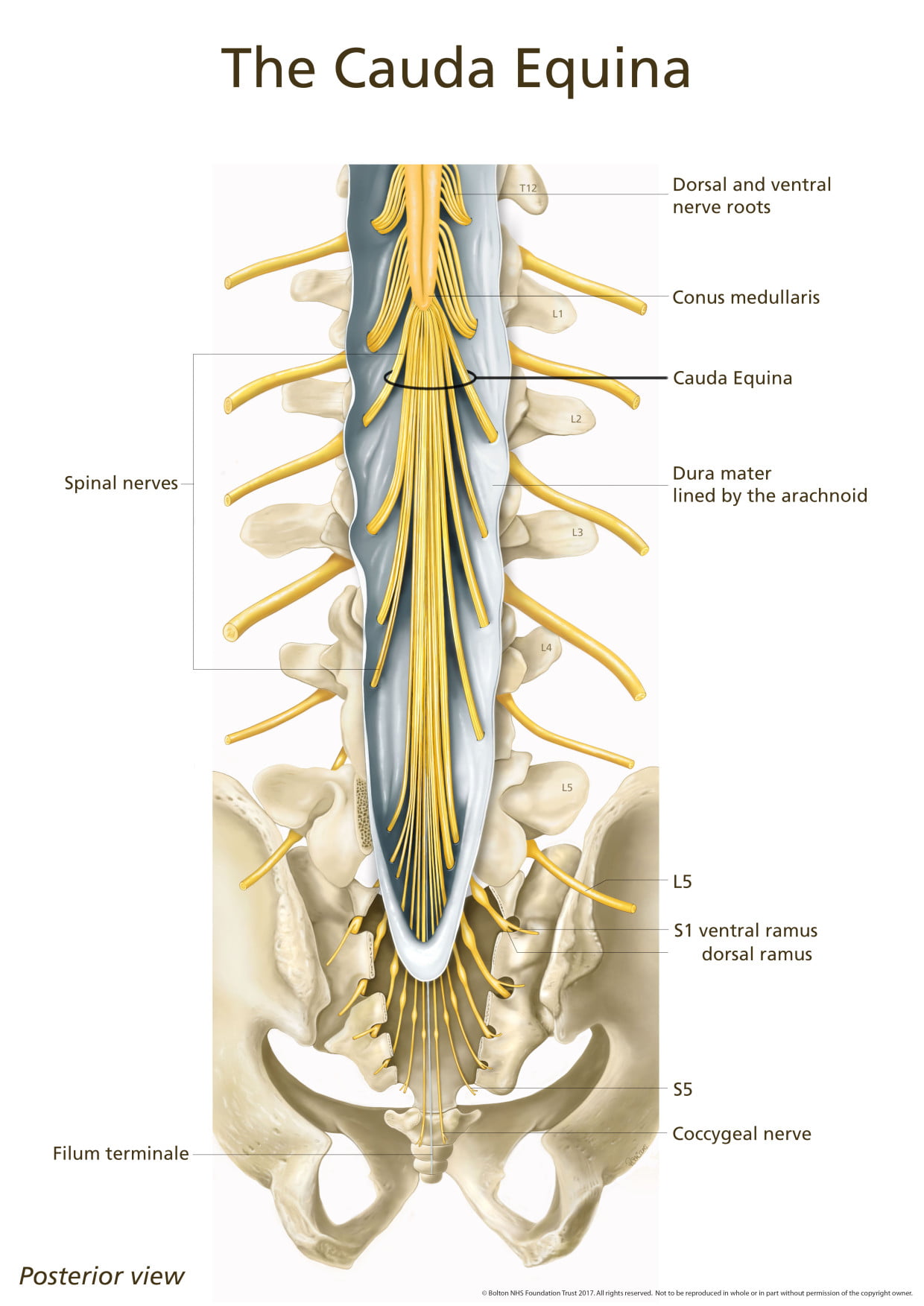
Neurologic Levels
Neurologic assessment should be made as soon as possible. Tonus (flaccidity, rigidity, spasticity) by passive movements is determined. Voluntary power of each suspected group of muscles against resistance is tested and the force compared bilaterally. Cremasteric (L1—L2), patellar (L2—L4), gluteal (L4—S1), suprapatellar, Achilles (L5—S2), plantar (S1—S2), and anal (S5—Cx1) reflexes are evaluated. Patellar and ankle clonus are noted. Coordination and sensation by gait, heel-to-knee and foot-to-buttock tests, and Romberg’s station test are checked.
Tenderness
Tenderness is frequently found at the apices of spinal curves and not infrequently where one curve merges with another. Tenderness about spinous or transverse processes is usually of low intensity and suggests articular stress. Tenderness noted at the points of nerve exit from the spine and continuing in the pathway of the peripheral division of the nerves is a valuable aid in spinal analysis pointing to a foraminal lesion. However, the lack of tenderness is not a clear indication of lack of spinal dysfunction. Tenderness is a subjective symptom influenced by many individual structural, functional, and psychologic factors that can make it an unreliable sign. An area for clues sometimes overlooked is the presence and symmetry of lower-extremity pulses.
LUMBAR SUBLUXATION SYNDROMES
Functional revolts associated with subluxation syndromes can manifest as abnormalities in sensory interpretations and/or motor activities. These disturbances may be through one of two primary mechanisms: direct nerve disorders or of a reflex nature.
Nerve Root Insults
When direct nerve root involvement occurs on the posterior root of a specific neuromere, it expresses as an increase or decrease in awareness over the dermatome; ie, the superficial skin area supplied by the segment. Typical examples include foraminal occlusion or irritating factors exhibited clinically as hyperesthesia, particularly on the:
(1) anterolateral aspects of the leg, medial foot, and great toe, when involvement occurs between L4 and L5 and
(2) posterolateral aspect of the lower leg and lateral foot and toes when involvement occurs between L5 and S1.
In other instances, nerve root involvement may cause hypertonicity and the sensation of deep pain in the muscles supplied by the neuromere. For example, L4 and L5 involvement, with deep pain or cramping sensations in the buttock, posterior thigh and calf, or anterior tibial muscles. In addition, direct pressure over the nerve root or its distribution may be particularly painful.
| Review the complete Chapter (including sketches and Tables) at the ACAPress website |



This book written by Dr. Richard C. Schafer is excellent. This is a must read for all Chiropractors.
Thanks Doctor Mike.
The clinical information in this book is invaluable. I do believe that the treatment protocols are now dated, and have been eclipsed by Liebenson’s active care protocols, as described in his Rehabilitation of the Spine: A Practitioner’s Manual.
Sometimes when I see someone and they get no results after adjusting their lower spine or SI joints, I check the cranials and the nervous system clears out and they get the results. Has anyone experienced these results.
Wow! What a wealth of information. I prefer this level of detail when trying to understand medical issues. I recently picked up a book called Surgery not Included by Dr. Richard E. Busch III which discusses treatment options for back pain relief. It really helped me to understand what back pain treatments to discuss with my parents doctor. Before we make a decision, we want to know ALL our options.
Dr. Marco
Do you have any friends who specialize in upper cervical? I’ve seen patients who’s low back issues resolved with UC work, but much more often I see it resolve with SI and infrequent lumbar adjusting.
Hi Betty
Dr. Shaffer was the most published chiropractic author (he passed away in 2001), and yes, his books are very in-depth. You might also review our Low Back Pain page, as it details how effective chiropractic is.
http://www.chiro.org/LINKS/lowback.shtml
[…] Lower Back Trauma. The following is Chapter 12 from RC’s best-selling book: “Chiropractic Posttraumatic Rehabilitation” […]
Discovering this site, I was shocked by the depth of info. Thanks
I think this is a good blog, very different and interesting.
This chapter everyone should read about every different condition relating to lower back pain is discussed in great detail.