Importance of the Type of Provider Seen
Importance of the Type of Provider Seen to Begin Health Care for a New Episode Low Back Pain: Associations with Future Utilization and Costs
SOURCE: J Eval Clin Pract. 2016 (Apr); 22 (2): 247–252
Julie M. Fritz PhD PT FAPTA, Jaewhan Kim PhD, and Josette Dorius BSN MPH
Department of Physical Therapy,
College of Health,
University of Utah,
Salt Lake City, UT, USA.
| Editorial Comment
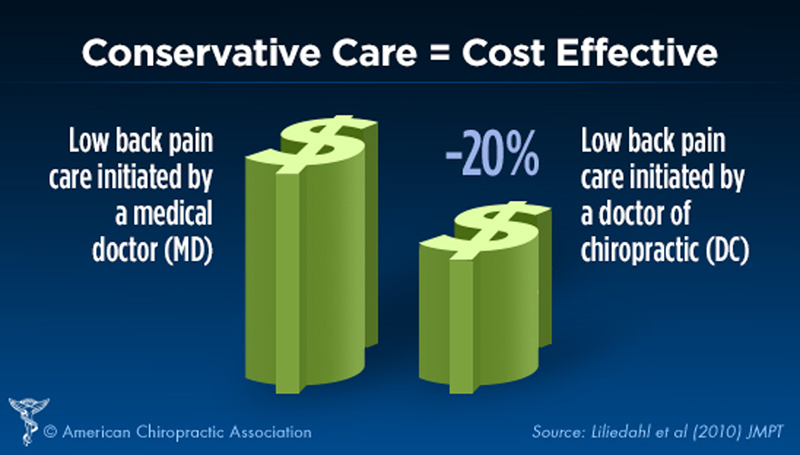
The RESULTS portion of this Abstract only partially discusses the findings, comparing 3 different professions’ treatment, costs, and outcomes for low back pain. In it they only mention the costs associated with medical management, while in reviewing chiropractic care vs. physical thereapy portions, they choose to emphasize:
That *seems* to suggest that physical therapy *may* entail less expense, or shorter durations of care, or that chiropractic patients are more likely to end up with surgery. None of that is true. Their own Table 2 plainly reveals that chiropractic care was the least expensive form of care provided to the 3 groups.
|