Addressing The Burden Of Spine-Related Disorders Through Integrated Value-Based Care
SOURCE: Health Affairs Forefront, February 12, 2025
Ryan Burdick • Christian Péan Sara • Holleran Inga Morken • Christine Goertz
Faculty of Health Sciences,
Ontario Tech University.

Editor’s Note:
This article is the latest in the Health Affairs Forefront series, Accountable Care for Population Health, featuring analysis and discussion of how to understand, design, support, and measure patient-centered, cost-efficient care under the umbrella of accountable care. Readers are encouraged to review the Call for Submissions for this series. We are grateful to Arnold Ventures for their support of this work.
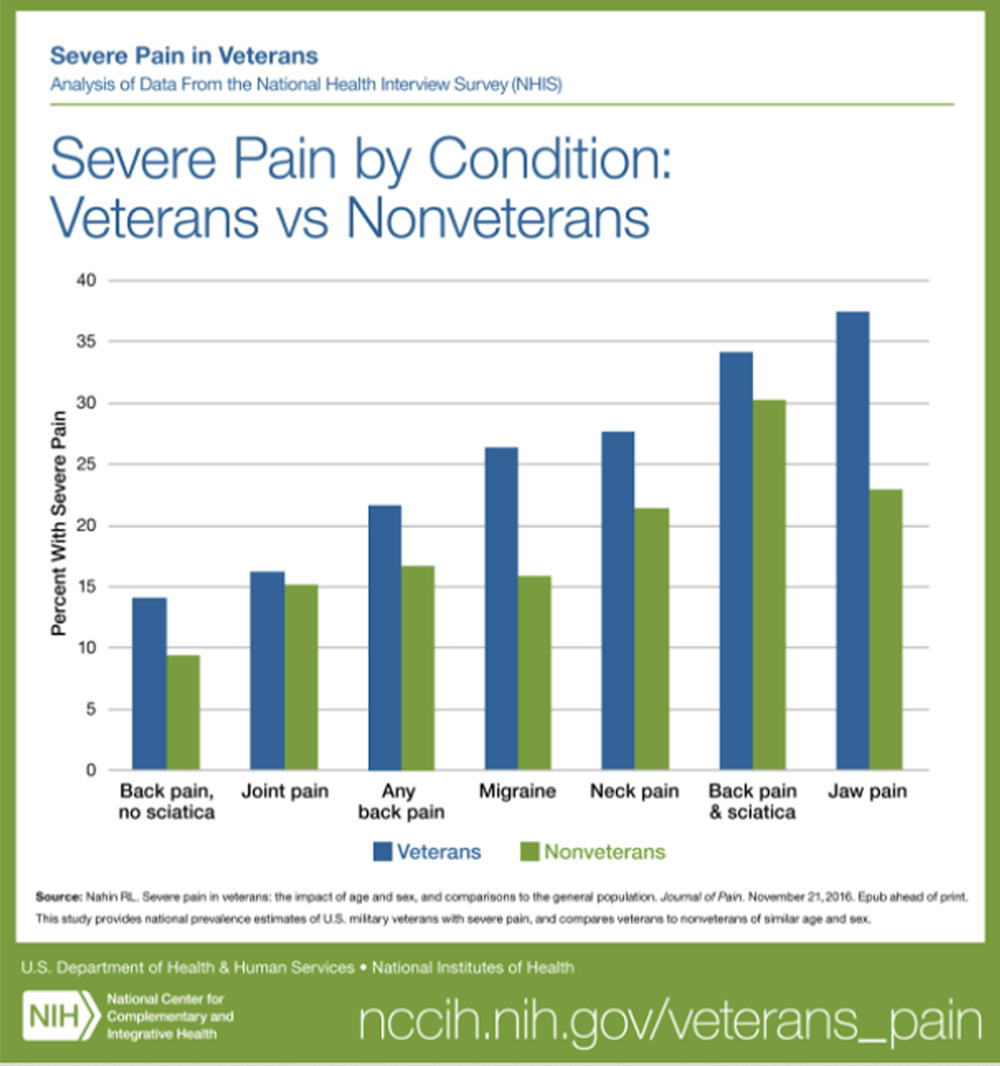
The unsustainable rise of health care costs in the US, coupled with suboptimal health outcomes, is driving both conversation and real action toward value-based care (VBC) models in this country. There is no more low-hanging fruit for this effort than spine-related disorders. Low back and neck pain cost us more than $134 billion annually and continues to rise at a rate more than twice that of overall health spending despite the fact that it is already at or near the top of all direct health care expenditures.
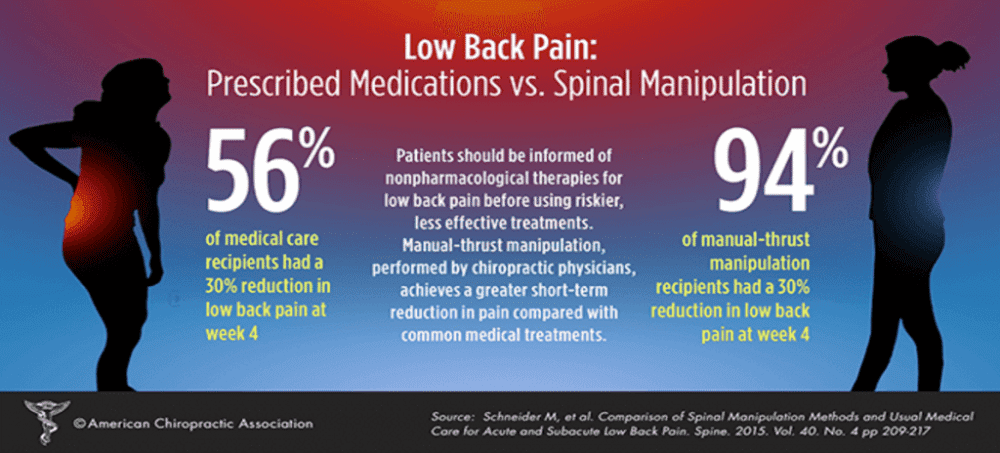
Despite aggressive and often invasive treatment approaches, low back pain remains the leading cause of physical disability worldwide with neck pain not far behind. This divergence between cost and outcomes is driven largely by the sustained use of expensive and ineffective treatments that can lead to more harm than benefit. Overreliance on prescription opioids began in the early 2000s, based on weak evidence suggesting that these medications were safe and effective treatments. In addition, the US maintains a higher rate of surgical interventions, more frequent specialist consultations for initial diagnoses, and consistently higher use of medically unnecessary advanced imaging.
Recognizing the profound impact of spine-related disorders, organizations including the
American College of Physicians, the
There is more like this @ our
INTEGRATED HEALTH CARE Section and the
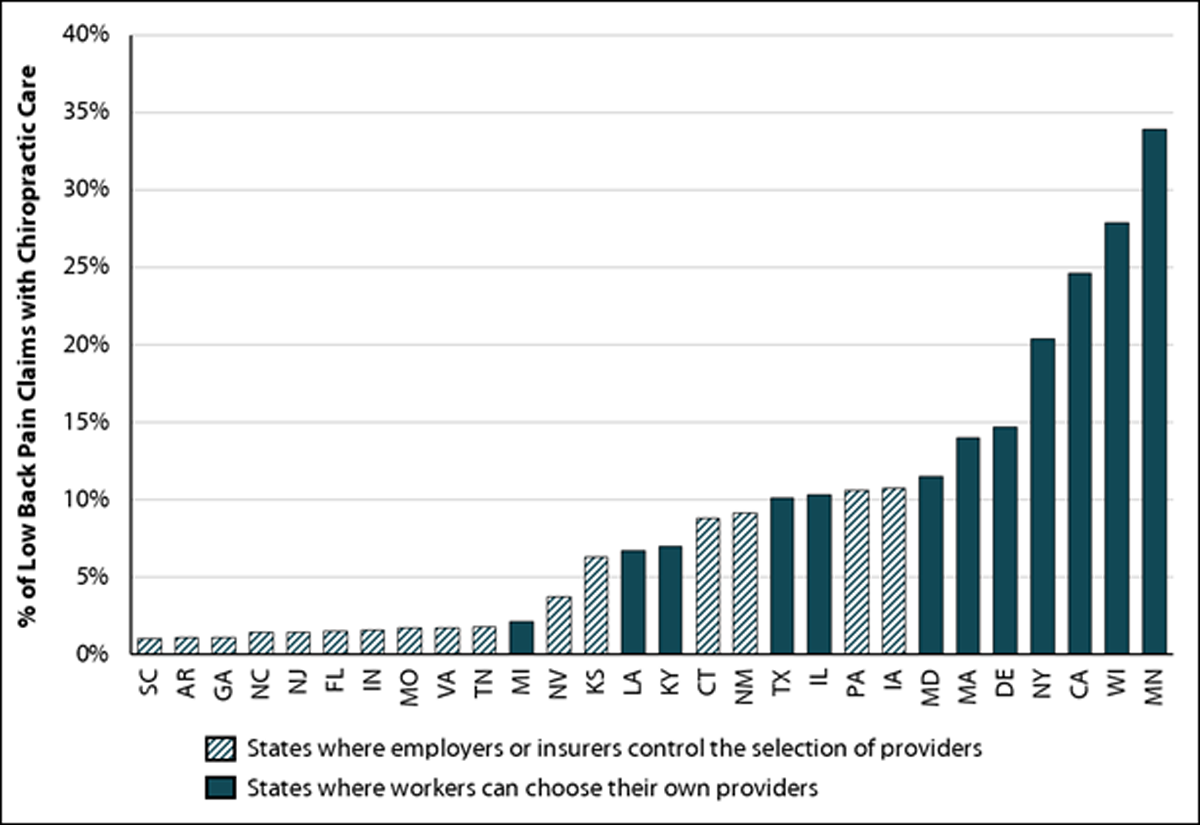
have all advocated for evidence-based, nonpharmacological treatment strategies for low back pain. These approaches emphasize conservative care as the first line of treatment, with invasive interventions reserved for cases in which patients do not improve with initial measures. However, adherence to guidelines remains poor, reflecting a systemic misalignment of incentives and care priorities in spine care.
A shift from fee-for-service care to value-based models would correct the perverse incentives that currently undermine optimal treatment of spine-related conditions. Such a transition could prioritize outcomes, reduce the overuse of low-value services, and incentivize the integration of multidisciplinary and evidence-based approaches. To date there is limited funding from government agencies for this effort and a lack of industry initiatives to explore what a value-based, population health-focused framework for treating spine-related disorders would entail. However, there are signs of movement in this direction. For example, the Center for Medicare and Medicaid Innovation (Innovation Center) recently rolled out a strategy to support person-centered, value-based specialty care to begin addressing the issues with fee-for-service care. Nevertheless, more work is needed. In this article, we outline the pressing need to build upon this and other existing VBC models for a range of disease conditions to directly target the delivery of evidenced-based spine care within a value setting.


Leave A Comment