Back and Neck Pain: In Support of Routine Delivery of Non-pharmacologic Treatments as a way to Improve Individual and Population Health
SOURCE: Translational Research 2021 (Apr 24);
| OPEN ACCESS |
Steven Z George, Trevor A Lentz, Christine M Goertz
Department of Orthopaedic Surgery and
Duke Clinical Research Institute,
Duke University,
Durham, North Carolina.
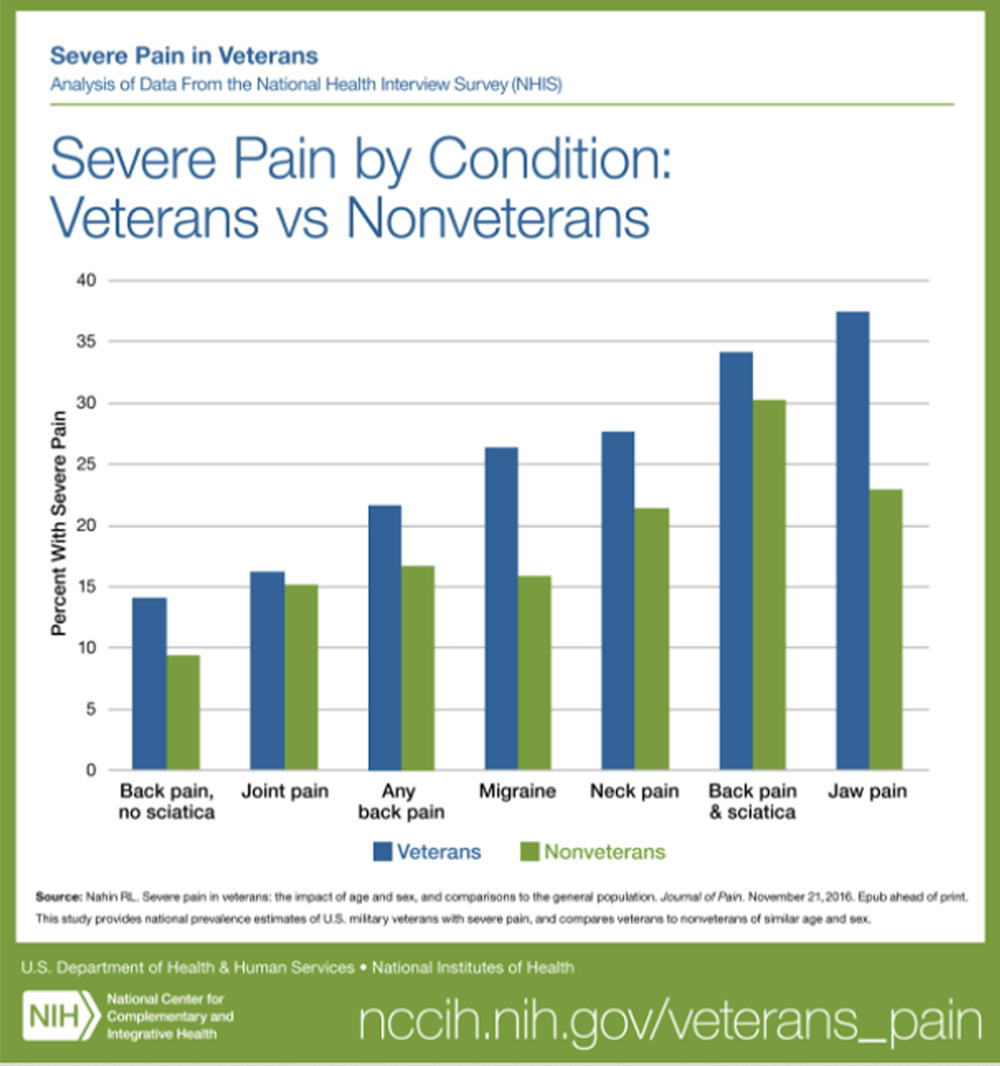
Chronic back and neck pain are highly prevalent conditions that are among the largest drivers of physical disability and cost in the world. Recent clinical practice guidelines recommend use of non-pharmacologic treatments to decrease pain and improve physical function for individuals with back and neck pain. However, delivery of these treatments remains a challenge because common care delivery models for back and neck pain incentivize treatments that are not in the best interests of patients, the overall health system, or society. This narrative review focuses on the need to increase use of non-pharmacologic treatment as part of routine care for back and neck pain.
First, we present the evidence base and summarize recommendations from clinical practice guidelines regarding non-pharmacologic treatments. Second, we characterize current use patterns for non-pharmacologic treatments and identify potential barriers to their delivery. Addressing these barriers will require coordinated efforts from multiple stakeholders to prioritize evidence-based non-pharmacologic treatment approaches over low value care for back and neck pain. These stakeholders include patients, health care providers, health care organizations, administrators, payers, policymakers and researchers.
There are more articles like this @ our brand new:
From the FULL TEXT Article:
INTRODUCTION
Chronic back and neck pain are highly prevalent conditions that are among the largest drivers of physical disability and cost in the world. [1] In fact, back and neck pain accounted for $134.5 billion of U.S. health care spending in 2016,2 This was the highest health care spending for any of the 154 medical conditions included in the study, led by private insurance (57.2%), then public insurance (33.2%), and out of pocket payments (9.2%). [2]The majority of physical disability and cost is associated with chronic back and neck pain conditions, which are the focus of this review.
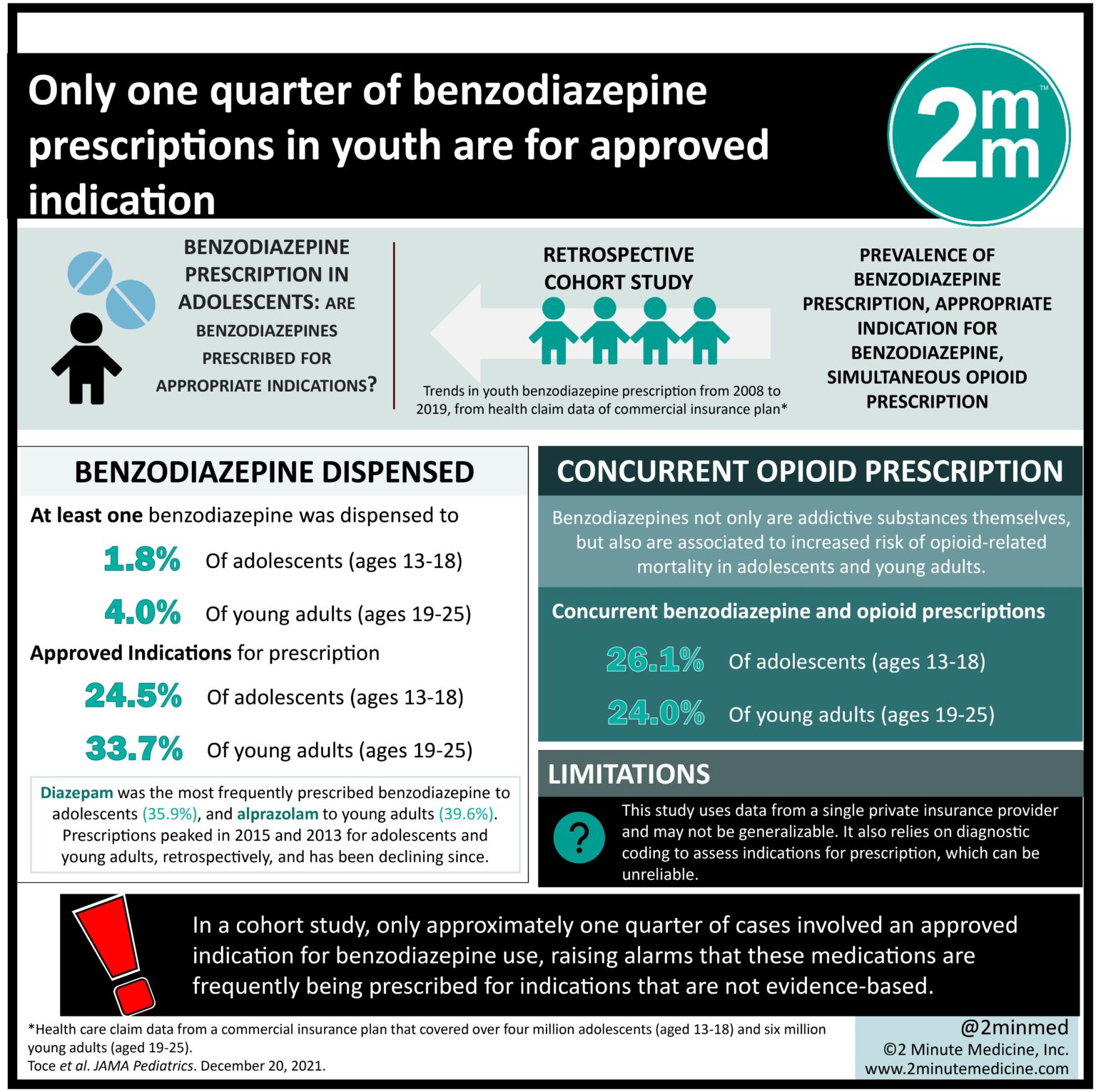
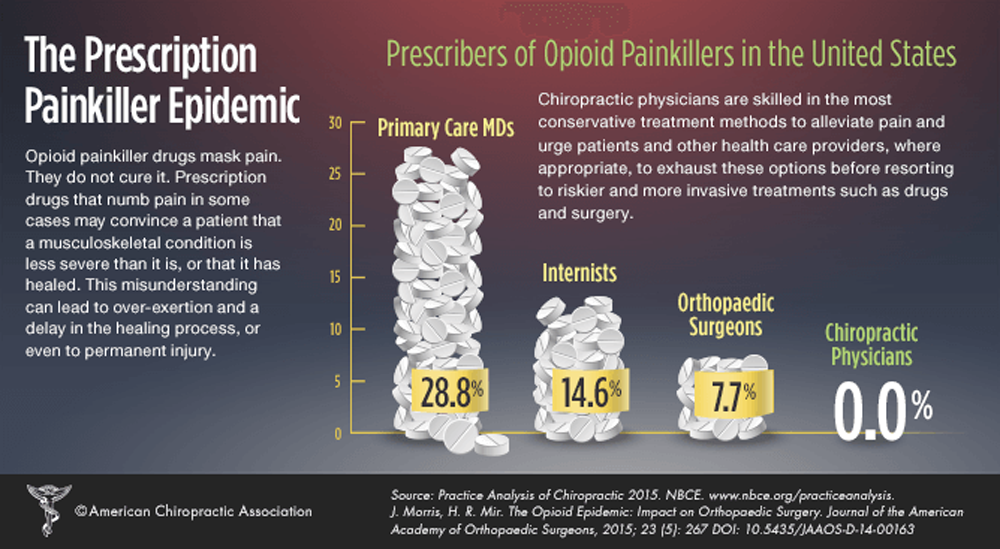
Traditionally, most care for back and neck pain begins with a patient visiting a primary care provider. [3] For decades, usual medical care for spine pain (whether an acute or chronic condition) has focused on standard treatments and technologies prescribed by primary care providers or procedures that require referral. Recently the effectiveness of this medically driven approach has been questioned in the literature. [4] Further, increasing evidence indicates that prescription medicine such as non-steroidal anti-inflammatory drugs and opioids, radiological/advanced imaging techniques, and invasive therapies such as spinal fusion and epidural injections have risks that can outweigh benefits to individual patients. [4]
Read the rest of this Full Text article now!



Leave A Comment