Integrating a Multidisciplinary Pain Team and Chiropractic Care in a Community Health Center
SOURCE: Journal of Primary Care & Community Health 2020 (Sep 10) ~ FULL TEXT
Christopher Prater 1, Melissa Tepe 2, Patrick Battaglia 3
Affiliations
1. Washington University School of Medicine, St. Louis, MO, USA.
2. Affinia Healthcare, St. Louis, MO, USA.
3. Logan University, Chesterfield, MO, USA.
Background: Chronic spinal pain is one of the most common diseases in the United States. Underserved patients are most affected, and disproportionately may use opioid medications as they lack access to other therapies. It is therefore important to develop systems to treat spinal pain within the primary medical home.
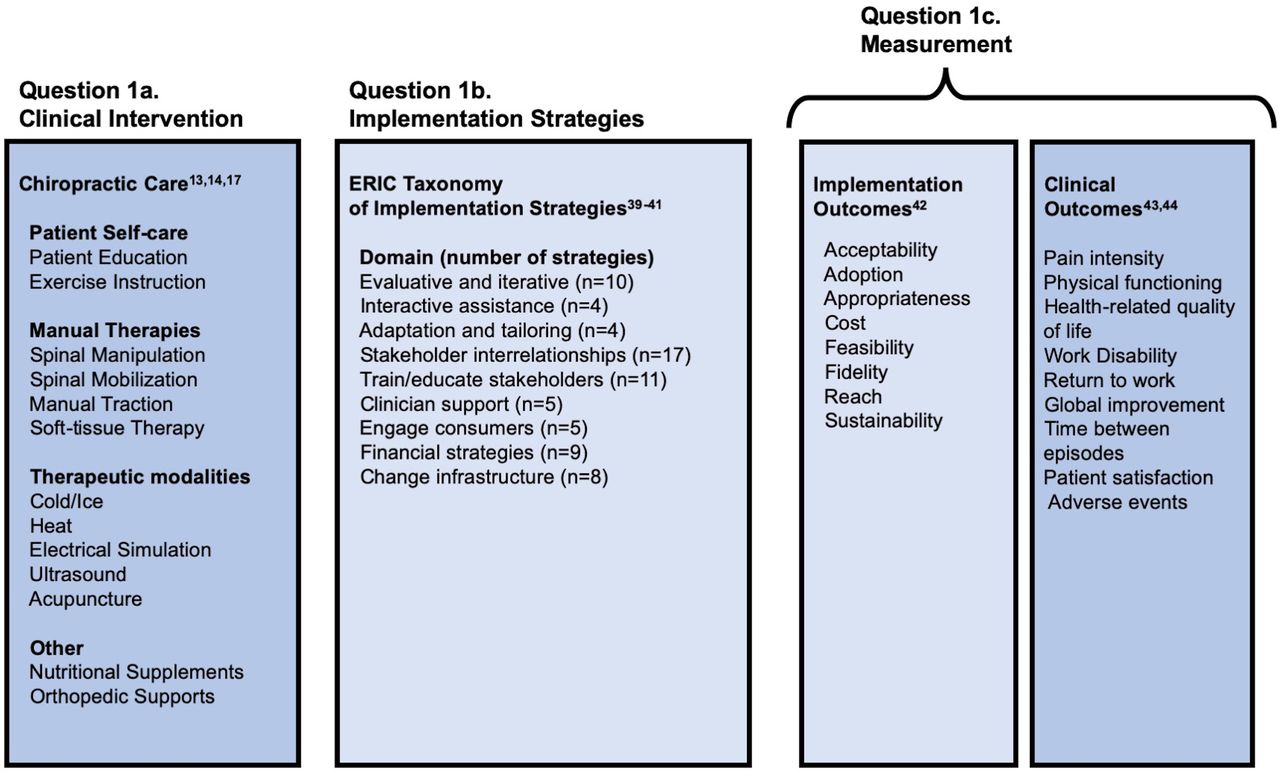
Methods: We designed a prospective observational pilot study at a community health center to measure the effectiveness of two interventions among an underserved population: a multidisciplinary pain team and chiropractic care. Study outcomes were pain and functional disability measured by the Pain Disability Questionnaire (PDQ), and reduction of opioid dose at baseline and 6–12 months. Multivariate linear regression was used to determine associating factors for change in PDQ scores.
Results: Thirty-five individuals completed baseline and follow-up PDQs from August 2018 to May 2020. Overall, the mean baseline PDQ was 92.4 +/– 6.1 and the mean follow-up PDQ was 81.9 +/– 7.7, resulting in a mean improvement of 10.6 (95% CI 1.2 – –22.3, P = .08). Participants in the chiropractic team (mean change –25.0, P = .01) and those completing the study before COVID-19 (mean change = –22.6, P < .01) were found to have significantly greater improvement at follow-up.
There are more articles like this @ our:
Conclusion: This observational study within a community health center resulted in improvement in spinal pain and disability with chiropractic care versus a multidisciplinary pain team. Offering similar services in primary care may help to address pain and disability, and hopefully limit external referrals, advanced imaging, and opioid prescriptions.
Keywords: integrated care; pain mangement; primary care; spinal pain; underserved communities.
From the FULL TEXT Article:
Introduction
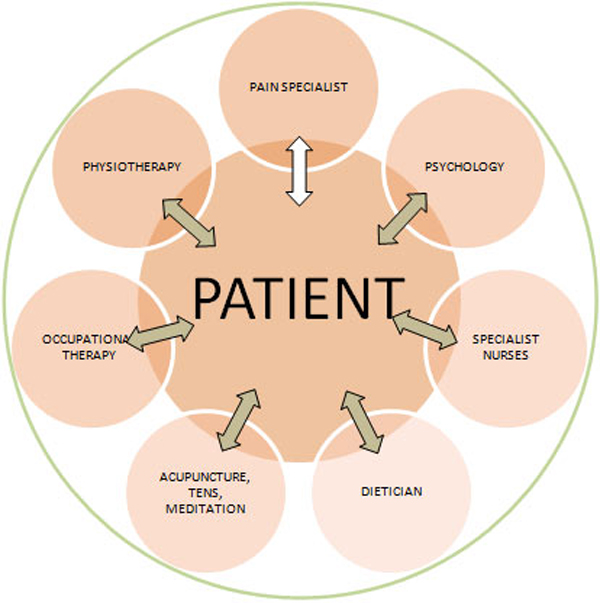
In the United States, 20.4% (50.0 million) adults suffer from chronic pain, and 8.0% (19.6 million) of U.S. adults have high-impact chronic pain (chronic pain limiting life and work activities). [1] Spinal pain is common and impactful, as low back pain is the first and neck pain is the fourth most common cause of years lived with disability globally, according to the Global Burden of Disease Study in 2010. [2, 3] Chronic pain is a biopsychosocial condition, and those medically underserved are at greater risk. Using the nationally-represented Health and Retirement Study, investigators determined that 17% of those living in the lowest wealth quartile suffer from high-impact chronic pain compared to 8% of the total study population. [4] Recent regional publications indicate 50%–60% of patients within Federally Qualified Health Centers (FQHCs) in the Midwest suffer from chronic pain. [5, 6] Furthermore, psychosocial variables such as depression, anxiety, and distress, which are common in underserved patients, mediate the transition from acute to chronic pain, and amplify existing pain complaints. [7, 8]
Patients with high-impact chronic spinal pain use opioids at a rate almost four times that of those with low-impact pain, and on average use over five times the morphine equivalent dose (MED). [9] The opioid epidemic has necessitated integrating safe, effective, and evidence-based treatments into chronic pain management, as prescription opioids have lacked efficacy and contributed to adverse effects and deaths. [10–12 ]American College of Physicians guidelines recommend non-pharmacologic (e.g. therapies routinely provided by chiropractors and physical therapists) and non-opioid pharmacologic treatment for low back pain, but high out-of-pocket expenses create access barriers to these evidence-based therapies for many low-income patients. [13–15 ] Average out-of-pocket expenses for one episode of low back pain can range between $150–720 for chiropractic or physical therapy with commercial healthcare insurance, and much greater without insurance. [14] In contrast, a one-month supply of generic opioids costs $10–15. [13]
Treatments provided by chiropractors are safe and effective in managing spinal pain, resulting in lower pain scores and increased patient satisfaction with minimal adverse events. [5, 21–25 ] Integrating chiropractic care in a low-income, urban clinic in Winnipeg, Canada not only reduced spinal and extremity pain, but also decreased opioid use. [20] There is also a foundation for on-site integration for pain management at the primary care level within the community health center (CHC), with proven feasibility and patient satisfaction, and opportunity for inter-professional collaboration. [5, 21–25 ] However, there are few quantitative studies of pain management integration into CHCs.
Our study site had recently implemented a multidisciplinary chronic pain team and chiropractic care to improve pain management and offer patients non-opioid treatments. Thus, we designed an observational study at a CHC with two distinct chronic pain interventions to determine the impact on treatment of chronic spinal pain and disability
There are more articles like this @ our:




Leave A Comment